Christiana Care Health System — rated No. 1 in the nation for medical excellence in stroke and neurological care by the CareChex Quality Rating System — participated in a groundbreaking research study that is redefining stroke treatment guidelines used by hospitals all across the country.
Neurointerventional doctors can now treat patients up to 24 hours after a stroke begins using a revolutionary brain imaging software to determine viability of brain tissue. This significantly widens the window for care that once closed at six hours.

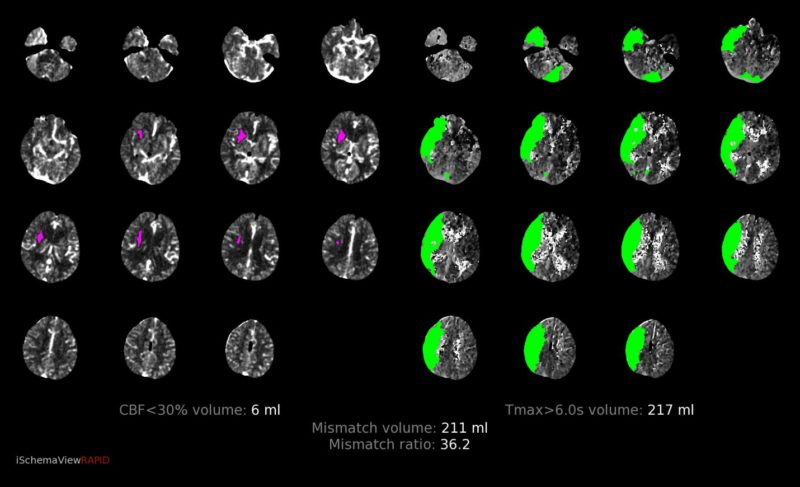
In two recent trials, the highly reliable, fully automated RAPID CT perfusion brain imaging software was proven to help neurointerventional specialists accurately determine whether a patient still has enough salvageable brain tissue to benefit beyond conventional time frames from a minimally invasive procedure called mechanical thrombectomy to remove the blood clot that is causing the stroke.
The results of these trials using RAPID CT Perfusion were so compelling that the American Heart Association / American Stroke Association recently released new guidelines extending the window for life-saving mechanical thrombectomy treatment from six hours up to 24 hours. Within four and a half hours of symptom onset, the intravenous (IV) clot-busting drug alteplase continues to be the first line of treatment. However, in the most severe strokes, IV alteplase is often not enough to restore blood flow to the brain, and many of these patients still benefit from mechanical thrombectomy.
The news is particularly important for patients who experience what is called a “wake-up stroke.” These are the patients who seem fine before bed (what stroke specialists call the “last seen normal”), but wake up more than six hours later with stroke symptoms such as drooping face, numbness or weakness on one side or difficulty speaking. Without knowing when the stroke actually began, and before the benefits of RAPID brain imaging, neuro specialists had limited reliable information to weigh the benefits versus risks of mechanical thrombectomy.
Christiana Hospital is the only comprehensive stroke center between Philadelphia and Baltimore — and the only hospital in Delaware — to offer this life-improving and sometimes life-saving procedure.
Feeding a catheter to the blocked vessel in the brain through the arm or leg, surgeons are able to grab a clot and pull it out mid-stroke — now up to 24 hours after symptom onset.

Barbara J. Albani, M.D., medical director of the Department of Neurointerventional Surgery, said RAPID imaging helps her team identify patients who could benefit from the minimally invasive therapy.
“Nothing is 100 percent, but RAPID gives us a better idea about which patients would benefit from clot removal and allows us to expand the time window to treat a broader group of patients,” she said.
The DAWN of a new era in stroke care
Neurointerventional specialists have had CT perfusion and imaging capabilities for years, but the core issue, said neurointerventional surgeon Thinesh Sivapatham, M.D., was figuring out what amount of brain tissue was permanently injured and what was salvageable. The old imaging tests sometimes offered good information, he said, but they were slow, labor-intensive and, most importantly, not reliable.
Aided by data from comprehensive stroke centers across the country (including Christiana Care), two recent landmark randomized controlled studies — the DAWN and DEFUSE 3 trials — present strong, clear benefits for patients who meet criteria for mechanical thrombectomy beyond the traditional six-hour treatment window thanks to RAPID CT perfusion.

DEFUSE 3 found that when patients are carefully selected using RAPID CT perfusion, mechanical thrombectomy is highly effective from six to 16 hours after the patient was last seen normal. DAWN showed that use of RAPID widens the treatment window for mechanical thrombectomy to as many as 24 hours. Both are monumental news for patients who wake up with stroke symptoms that likely originated well beyond the traditional six-hour treatment guidelines.
“Before the DAWN and DEFUSE 3 trials, we did not have a fast, safe and reliable way to choose patients for treatment,” he said. “Now we do.”
The automated RAPID CT perfusion software is consistent, high quality and very fast — hence the name RAPID.
Said Dr. Sivapatham, “With RAPID, the information we need to make better-informed treatment decisions is on our phones in two or three minutes.”
Right care, right place, right time
Without cutting-edge imaging platforms like RAPID CT perfusion and therapies like IV alteplase or mechanical thrombectomy to stop a stroke in its course and restore blood flow to the brain, patients may be left bedridden. When blood flow is restored to viable brain tissue, patients often begin talking and moving limbs right on the treatment table in the interventional suite.
“To have such a drastic improvement in patients so quickly is what drives us to do the best we can and stay on top of current guidelines,” said Dr. Sivapatham.
Participation in national guideline-changing trials such as DAWN — and staying on the cusp of cutting-edge changes in stroke care — are important responsibilities for Christiana Care. Christiana Hospital is one of only a select few in the country that the Joint Commission has designated a comprehensive stroke center, where patients can receive the highest level of stroke care, including life-saving neurointerventional and neurosurgical procedures. Wilmington Hospital serves as a primary stroke center.
“As stroke care leaders in our community, we keep our fingers on the pulse of the latest technology, research and treatment options available, thereby giving our patients the best possible care,” said Dr. Albani. “It is our job and our duty to be on top of new opportunities to improve stroke care. It really does affect our neighbors and how we are able to treat patients.”
Christiana Care’s broad, multidisciplinary Stroke Center team includes members from the emergency department, stroke neurology, neurointerventional surgery, neurosurgery, neurointensive care, radiology, pharmacy and rehabilitation, as well as stroke program coordinators, nurses and patient care technicians. Stroke care begins in the field with emergency medical technicians who begin life-saving stroke treatment en route to the emergency department and alert the stroke team at Christiana Hospital that a patient is on the way. Stroke care may continue after the patient leaves the hospital, which is why a comprehensive approach to treatment is so important.
Christiana Care was a driving force in partnering with other hospitals in Delaware to develop legislation to create a statewide stroke care system. This allows patients anywhere in the state to get the best care possible both locally and regionally. In some cases, severe stroke patients or critically ill patients are transported from hospitals throughout the state to Christiana Hospital, where the most advanced imaging capabilities, interventional/surgical treatments, neurointensive care and rehabilitation, are available 24 hours a day.
It’s all about getting patients to the right hospital at the right time for the best chance of recovery. Teams from each hospital, the emergency medical services community and rehabilitation facilities statewide meet quarterly to reassess what is the best care for the treatment of stroke patients across the state.
Time is brain
While the extended treatment window for stroke treatment dramatically increases the number of patients Christiana Care stroke specialists may able to help with mechanical thrombectomy, Drs. Albani and Sivapatham caution that it in no way means patients should take their time calling for help when they suspect a stroke.
Nearly two million neurons, or brain cells, die every minute that a clot blocks blood flow to the brain.
Said Dr. Sivapatham, “We have a saying, ‘Time is brain.’ We know for a fact that time is of the essence in stroke — the longer you wait to seek treatment, the chance of a good outcome is reduced minute by minute.”
Dr. Albani said she worries that many people don’t realize that a stroke is an emergency of the same degree as a heart attack. They ignore symptoms or wait to see if they will go away.
“For every 15 minutes of delay, you lose significant chance of good functional outcome,” said Dr. Albani. “Thanks to RAPID CT perfusion capabilities, we now are able to treat more patients further out from the onset of their stroke symptoms, but you still must get to the hospital as soon as possible.”
While not every patient will meet the strict criteria for mechanical thrombectomy beyond six hours, Doug Huisenga, MPT, ATC, Neuroscience program manager, said the information now available to specialists thanks to RAPID CT perfusion software gives more people a shot at recovery.
“We provide the best possible stroke care as fast, if not faster, than anybody in the nation,” he said. “We treat large numbers of patients with stroke every day — because when your life depends on it, experience matters.”
Stroke care timeline
At the moment a 911 call is received for a stroke, care teams rush into action. Here are some of the steps that take place:
- Delaware’s statewide Stroke Care System activates. EMS notifies Christiana Hospital of an incoming stroke patient.
- Christiana Hospital activates Stroke Alert, alerting the emergency department, stroke neurology and neurointerventional teams, as well as radiology/CT and pharmacy.
- Emergency medical technicians begin treatment in the ambulance or helicopter en route to the hospital.
- Pharmacy prepares IV alteplase (clot-busting drug).
- Patient is immediately assessed upon arrival to emergency department.
- Head CT is performed and quickly interpreted by a neuroradiologist.
- Patient immediately receives IV alteplase (clot-busting drug) if eligible.
- RAPID CT perfusion is performed to assess viability of brain tissue, as well as CT angiogram to identify vessel occlusion. Carefully selected patients are immediately moved to the neurointerventional suite for minimally invasive mechanical thrombectomy procedure, when appropriate.
- In the best cases, the patient often begins talking and moving limbs before leaving the operating room.



