As an acute care virtual nurse, Melanie Ries, RN, MEDSURG-BC, is never out of touch with her patients – even if she is working miles away from their bedside.
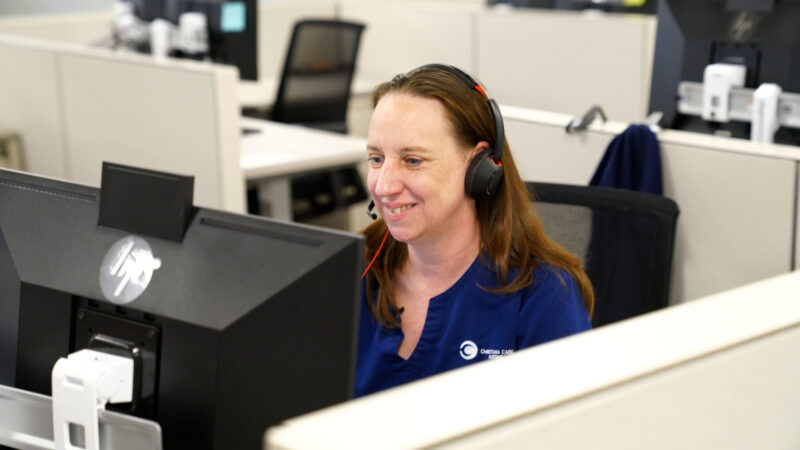
With a click of her mouse, she can securely monitor a patient’s vital signs, join the care team for multidisciplinary rounds and assist with admission and discharge planning.
A survey found that 78% of patients who used virtual nursing during their hospital stay liked it.
She’s also available for instant communication with patients who call her from a computer tablet in their hospital room to ask questions about their medication or have her speak with a family member.
Virtual nurses offer a critical extra set of eyes and connection that many health care leaders believe could help alleviate staffing shortages, assist the next generation work force and improve patient experience.
“We can fully focus on the patient in front of us and not have to worry about answering a call bell from another room. And because virtual nurses take away some of that documentation burden, we make it possible for those at the bedside to use their time in a way that’s more hands-on,” said Ries, who has been a nurse for 16 years. She spends part of her time office-based as a virtual nurse and the rest of her time in the hospital as a nurse seeing patients on their units.
ChristianaCare — a pioneer in virtual nursing

ChristianaCare is among a small but growing group of health care organizations helping to plot the future direction of virtual nursing.
Today, nearly 41% of ChristianaCare’s acute care beds have access to virtual nursing services and another 500 beds are planned later this year. In addition, ChristianaCare nursing leaders are working on the national level to advocate for policy development related to virtual nursing practice standards to the American Nurses Association.
“We really see virtual nursing as an opportunity to evolve the care delivery model and also potentially impact practice among other disciplines,” said Michelle Collins, DNP, APRN, CNS, ACNS-BC, NPD-BC, NEA-BC, LSSBB, who leads ChristianaCare’s systemwide efforts in nursing practice innovation as vice president for nursing professional excellence.
“This innovation allows nurses to practice at the highest levels while also contributing to shorter patient stays and enhancing outcomes,” Collins said.
ChristianaCare launched its virtual acute nursing program in September 2022 with a 49-bed pilot between a unit at Wilmington Hospital and another at Christiana Hospital.
Interested in a nursing career at ChristianaCare? Click here.
It didn’t take long to see the benefits of the program, Collins said. Both units saw improvements in patient satisfaction metrics. A separate survey found 78% of patients who used virtual nursing during their hospital stay liked it.
By June 2023 — less than six months later — the program had expanded to 510 beds across 17 units, accounting for 41% of all acute care beds in ChristianaCare’s Delaware hospitals. More than 19,000 patients received virtual nursing care, with over 53,000 calls handled between patients, families, other caregivers and virtual nurses.
‘Connection was fast’
For patient Gary Glick, the immediate access to a virtual nurse was another reason for him to feel comfortable during his acute care hospital stay.
“The connection was fast. The nurse was right on there and she was already versed in my situation, so it made the conversation a lot easier in my mind,” he said.
As ChristianaCare’s virtual nursing program grows, the connection it creates remains one of its greatest strengths.
“It’s the one-to-one relationship between the nurse and patient that makes a difference,” Collins said.
“There’s no interruption. There are no call bells going off. You’re not worried about hanging IV bags or a provider walking in to talk with you about the plan of care in another room.”
Expanding the virtual nursing model
As more programs look to develop their own virtual nursing programs, ChristianaCare has emerged as a national leader. Collins also has established a nationwide Virtual Acute Care Network with about 45 health care organizations participating.

Collins said she can see other disciplines in the future using the virtual nursing model to deliver care more efficiently.
“When our focus is on how we can make sure patients get the care they need and also make sure our workforce has the opportunities to practice in a more efficient and effective way, I think we can really create an experience that benefits both,” she added.
A culture of nursing innovation
ChristianaCare’s virtual acute care nursing program is housed within the Center for Nursing Innovation established in January 2023.
The center, headed by Collins, along with Jennifer Painter, DNP, CNS, associate chief learning officer and vice president of Nursing Professional Development; Susan Mascioli, MS, BSN, RN, NEA-BC, CPHQ, LSSBB, CPPS, vice president of Nursing Quality and Safety; and Katherine “Kat” Collard, MS, RN-BC, NP, chief nursing informatics officer, is a collaborative effort to drive and support new ideas, opportunities and transformations in nursing.

“The Center for Nursing Innovation is a non-brick-and-mortar entity encompassing the pillars of excellence, professional development, informatics and quality and safety within nursing,” Painter said.
In the past year, the center has hosted workshops to showcase nurse inventors in the system who have obtained patents, supported four teams that competed in the national NurseHack4Health and explored ways to relieve the documentation burden on nurses by using artificial intelligence.
“Whether you are a nurse practitioner, a nurse scientist, a clinical nurse, an ambulatory nurse or a home health nurse, you should have access to information, planning, professional development and evidence-based practices to help innovate your practice,” Collins said.
“We want to foster a culture within ChristianaCare where nurses who are coming across clinical scenarios have a place to explore problem-solving. Through our Center for Nursing Innovation, they can get help with how to apply an innovative thought process to a problem.”
“We are critically thinking about exceeding our care deliverables for excellence and leveraging what we know how to do as nurses.”
Nurses have a unique role, and that perspective offers great potential to tackling health care problems, especially when it involves using technology to reduce administrative burden, Collard said.
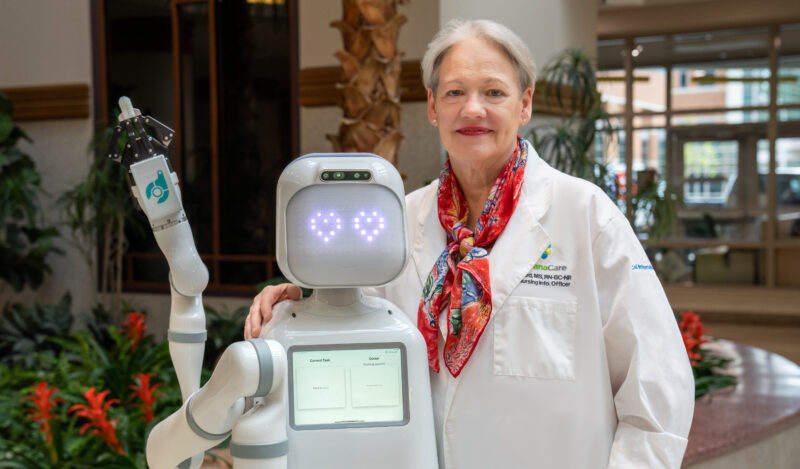
“We are moving away from the traditional efforts to think outside the box and transform the way we care for our patients,” Collard added.
The center offers support for nurses seeking help with project management and grant applications and those seeking a mentor or who want to explore another aspect of the profession, such as leadership or process improvement.
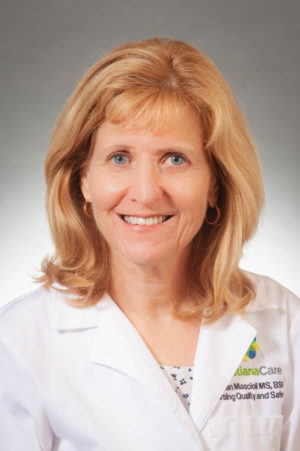
“We are working to embed innovative thinking and evidence-based practice changes among our nurses to make systemwide improvement,” Mascioli said.
‘Very rewarding’
Splitting her time between virtual nursing and working at the bedside, said Ries, has made a difference for her both professionally and personally.
“It’s definitely very rewarding when I work in the virtual space and I’m able to talk to a patient one on-one without all the distractions and the giant to-do list,” she said.
“And then when I work in the clinical space on the floor, I’m not as physically exhausted trying to keep up with everything.”
She also appreciates the overwhelmingly positive response from other health professionals. Ries said some providers will call the virtual nurse when they’re in with a patient, leading to a deeper conversation about the patient’s plan of care.
“One of the advantages of the virtual nursing model is the way it naturally integrates ChristianaCare’s values and behaviors, including anticipating the needs of others and looking for new ways to innovate,” Collins said. “It’s another way to serve with love and excellence while relieving the burden on other caregivers.
“I think that’s where the opportunity is – optimizing this program to that both virtual and clinical nurses leave at the end of their shift saying, ‘Today, I delivered exceptional care to my patients and families.’ We can do that,” she added.



