Researchers Find Disparities in Breast Cancer Screening in Delaware Linked to Race and Geography
First study of its kind concludes that data analytics should pinpoint locations for new mammogram screening sites

How easy is it for a woman to get a mammogram? The answer depends on whether she lives in an urban or a rural area, and it can vary widely based on the racial makeup of her community, according to a study co-authored by researchers from ChristianaCare’s Helen F. Graham Cancer Center & Research Institute and published in Breast Cancer Research.
In the first study of its kind, researchers found disparities in the location of mammography screening sites in Delaware.
“Ensuring equitable geographic access to screening mammography must be an important priority for reducing disparities in breast cancer outcomes,” said Scott Siegel, Ph.D., MHCDS, director of Cancer Control & Population Sciences at the Graham Cancer Center and the senior author on the paper.
In the first study of its kind, researchers found disparities in the location of mammography screening sites in Delaware.
“Our study had two objectives. Besides identifying where disparities in mammography screening exist, we went a step further to suggest what we might do to correct the issue, by pinpointing potential locations for additional screening sites,” Siegel said.
While the study focused on breast cancer in Delaware, the authors believe the research approach can be replicated in other states or geographic regions to help improve access to mammography and ultimately reduce breast cancer disparities.
The state of Delaware has an elevated burden from breast cancer but is otherwise representative of the U.S. in terms of race and urban/rural characteristics, making it a strong demographic base for this research.
Despite a 40% reduction in breast cancer mortality over the last 30 years in the U.S., not all groups have benefited equally from these gains. A consistent link between later stage of diagnosis and disparities in breast cancer mortality has been observed by race, socioeconomic status and rurality (defined by population density).
Catchment and ‘location-allocation’ analyses
The researchers first conducted a catchment analysis (proximity within driving distance) of existing mammography facilities. The study used an analytical tool to ascertain the geographic distribution of mammography sites and Breast Imaging Centers of Excellence (BICOEs) in Delaware and those in border-adjacent ZIP codes in Maryland and Pennsylvania. (The BICOEs have been recently renamed American College of Radiology Designated Comprehensive Breast Imaging Centers.)
The catchment analysis showed that for each standard deviation increase in the number of Black women in a census tract, there were 68% fewer mammography units and 89% fewer BICOEs.
The more rural counties in the state accounted for 41% of the population but only 22% of the BICOEs.
“Equitable geographic access to screening mammography must be an important priority for reducing disparities in breast cancer outcomes.”
— Scott Siegel, Ph.D.
Finding evidence of disparities by race and rurality, the researchers next conducted a “location-allocation” analysis to identify candidate locations for the establishment of new mammography facilities to optimize equitable access, following several sets of breast cancer screening guidelines.
The results of the location-allocation analysis depended on which set of screening guidelines were adopted, which included increasing mammography sites in communities with a greater proportion of younger Black women and in rural areas.
Targeting triple negative breast cancer
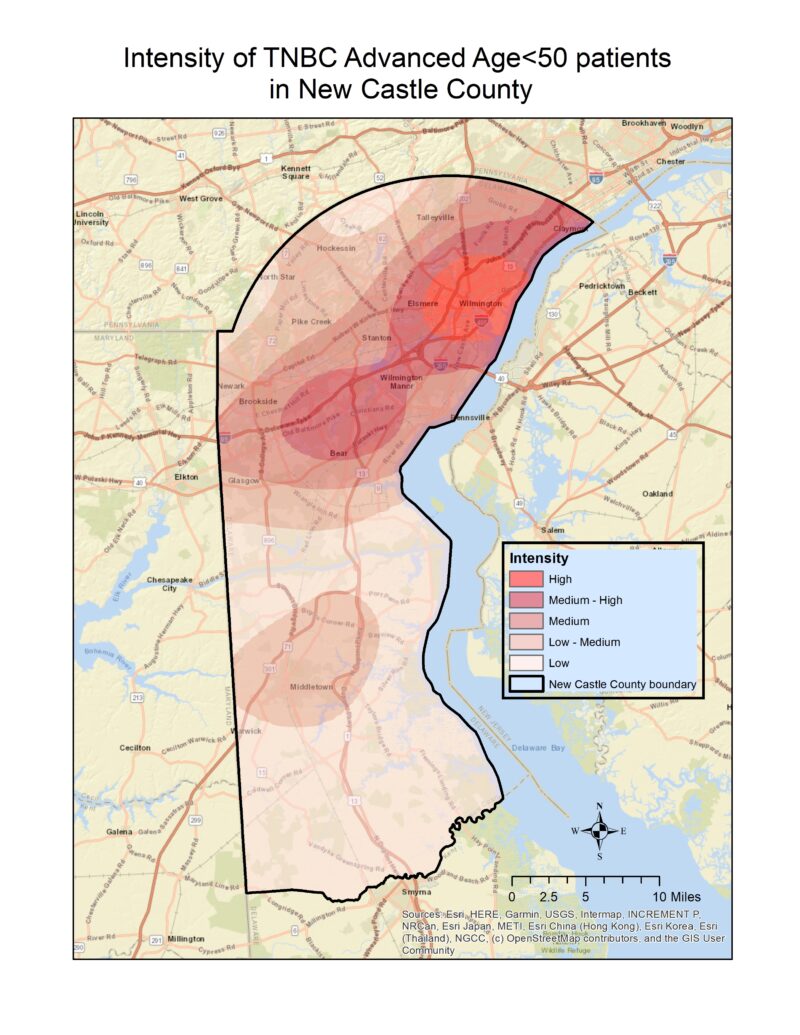
In the U.S., Delaware is number one for incidence of late-stage breast cancer among women under 50 as well as number one for incidence of an aggressive subtype known as triple negative breast cancer (TNBC) that disproportionately affects Black women and is more likely to present at a younger age. There is preliminary evidence that the benefits of screening mammography extend to early detection of TNBC.
The authors acknowledge that living in proximity to screening services does not equate to access for everyone. Their work continues to examine relationships between higher numbers of advanced cancer diagnoses and suboptimal mammography screening rates in communities where other potential disparities have been identified.
Siegel is also the lead author of a commentary published Nov. 1, 2023, in Population Health Management calling upon community members, health care providers and other stakeholders to collaborate to address disparities in breast cancer.
“By working together, we eliminated disparities in colorectal cancer across our state 10 years ago, and we can do it again with breast cancer,” he said.
“Our latest study illustrates that given a set of guidelines, the location and number of mammography facilities can be guided by catchment and location-allocation analytic tools as part of a larger strategy to close breast cancer disparities.”