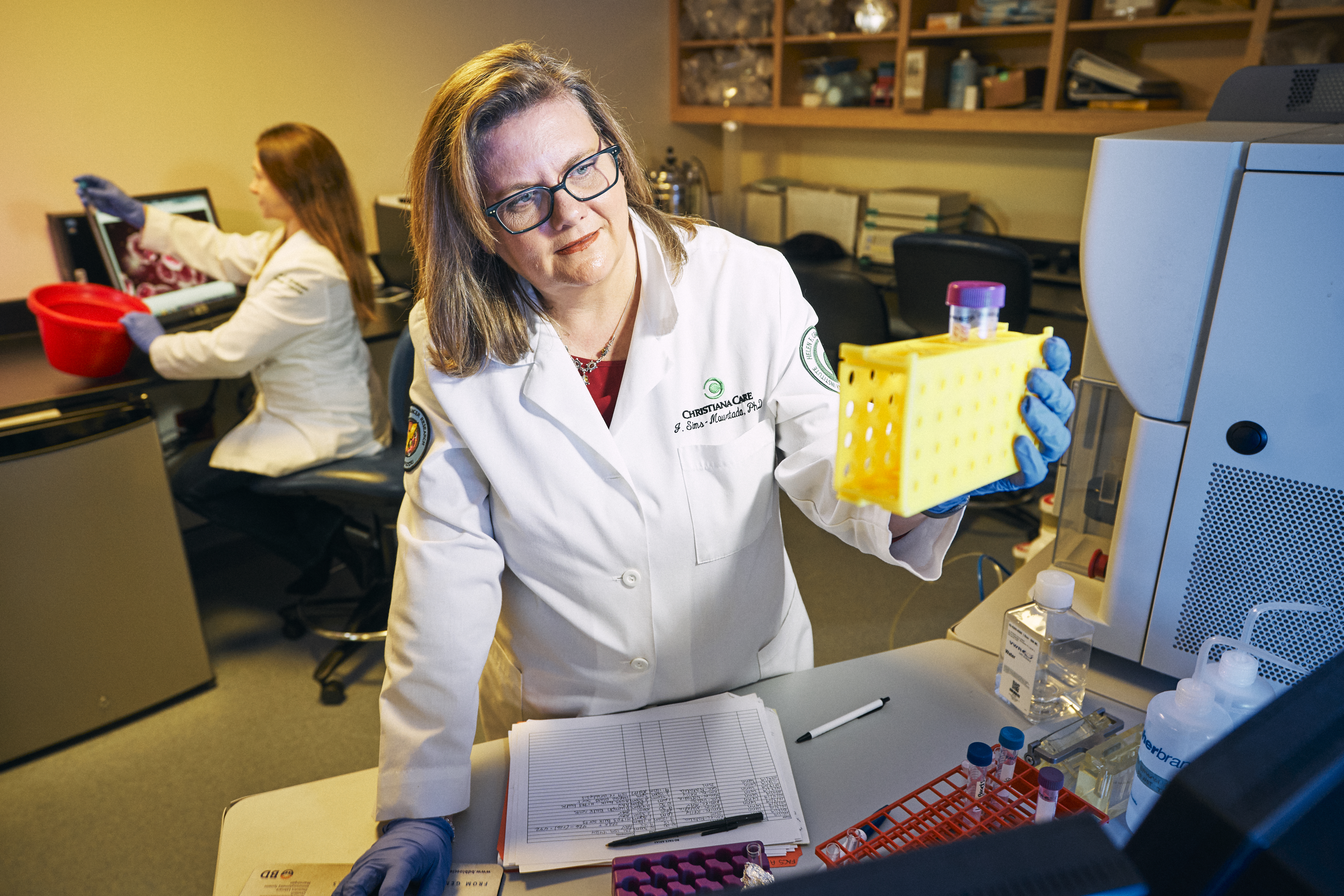
The Lisa Dean Moseley Foundation has awarded a $659,538 grant to further research on inflammation as a driver of triple-negative breast cancer to Jennifer Sims-Mourtada, Ph.D., director of Translational Breast Cancer Research at ChristianaCare’s Helen F. Graham Cancer Center & Research Institute.
The three-year grant will enable Dr. Sims-Mourtada and her team at the Center for Translational Cancer Research to continue investigating the role of cells immediately around a tumor in spurring the growth of triple-negative breast cancer and possible therapy for this particularly difficult cancer.
This cancer is resistant to current therapies and has significantly worse outcomes than other forms of breast cancer. It disproportionately affects premenopausal women and African-American women.
“The Moseley Foundation’s grant will help our breast cancer research team address a pressing concern for Delaware, which has the highest rate of triple-negative breast cancer in the nation,” said Nicholas J. Petrelli, M.D., Bank of America endowed medical director of the Helen F. Graham Cancer Center & Research Institute.

“Our multifaceted approach to cancer care, with its emphasis on community outreach and advanced research translating to new, more effective treatments, is all part of our commitment to being exceptional today and even better tomorrow on behalf of our patients.”
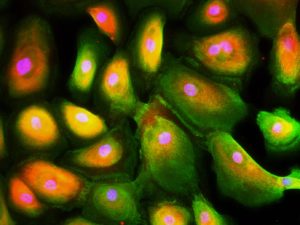
Triple-negative breast cancer is thought to arise from mammary stem cells that have mutated into cancer stem cells. Their abnormal growth capacity and survival mechanisms make them resistant chemotherapy.
Her previous research has shown that some of the body’s normal inflammatory responses, which usually are associated with wound healing, can instead promote tumor growth and resistance to treatment in triple-negative breast cancer.
During normal injury like a cut or scrape, lost skin cells are replaced by an expansion of normal stem cells, driven by potent growth factors released by immune cells at the wound site. The process continues until the wound is closed and the stem cells “turn off” and stop expanding.
In triple-negative breast cancer, these stem cells continue to expand. Also, they often are invisible to the immune system, and may even be able to suppress the immune system itself, preventing the body or chemotherapies from effectively fighting tumor growth.

“At the core, we’re looking at cancer stem cells, which are found in many different types of cancers, and how they resist treatment, ‘hide’ from the immune system and then keep growing back,” Dr. Sims-Mourtada said.
“If we can figure out how they are hiding and how we can activate the immune system to ‘see’ them again in breast cancer, then we can figure it out for other forms of cancer.”
The grant will help the research team investigate the relationship between cancer stem cells and immune cells to determine how inflammation may spur the growth of triple-negative breast cancer tumors.
The grant funds will enable the researchers to compare breast tissue from patients with the cancer before and after chemotherapy to identify whether resistant tumors have an inflammatory “signature” that would help flag the presence of cancer stem cells within them.
In previous research, Dr. Sims-Mourtada’s team identified an anti-inflammatory drug, currently used to treat rheumatoid arthritis, that has the potential to target and inhibit the growth of cancer stem cells and triple-negative breast cancer tumors.
They will use the grant to further study the drug’s effects — research that could set the stage for clinical investigation of the drug, alone or in combination with chemotherapy, to improve outcomes for patients with triple-negative breast cancer.
“The work of Dr. Sims-Mourtada and her team supports the Lisa Dean Moseley Foundation’s mission to encourage and promote stem cell research,” said William J. Martin, the foundation’s secretary-treasurer.
“By increasing the understanding of the effects chronic inflammation may have on stem cells, Dr. Sims-Mourtada and her colleagues have the potential to accelerate progress toward targeted, more effective treatments for triple-negative breast cancer and other inflammation-associated cancers.”