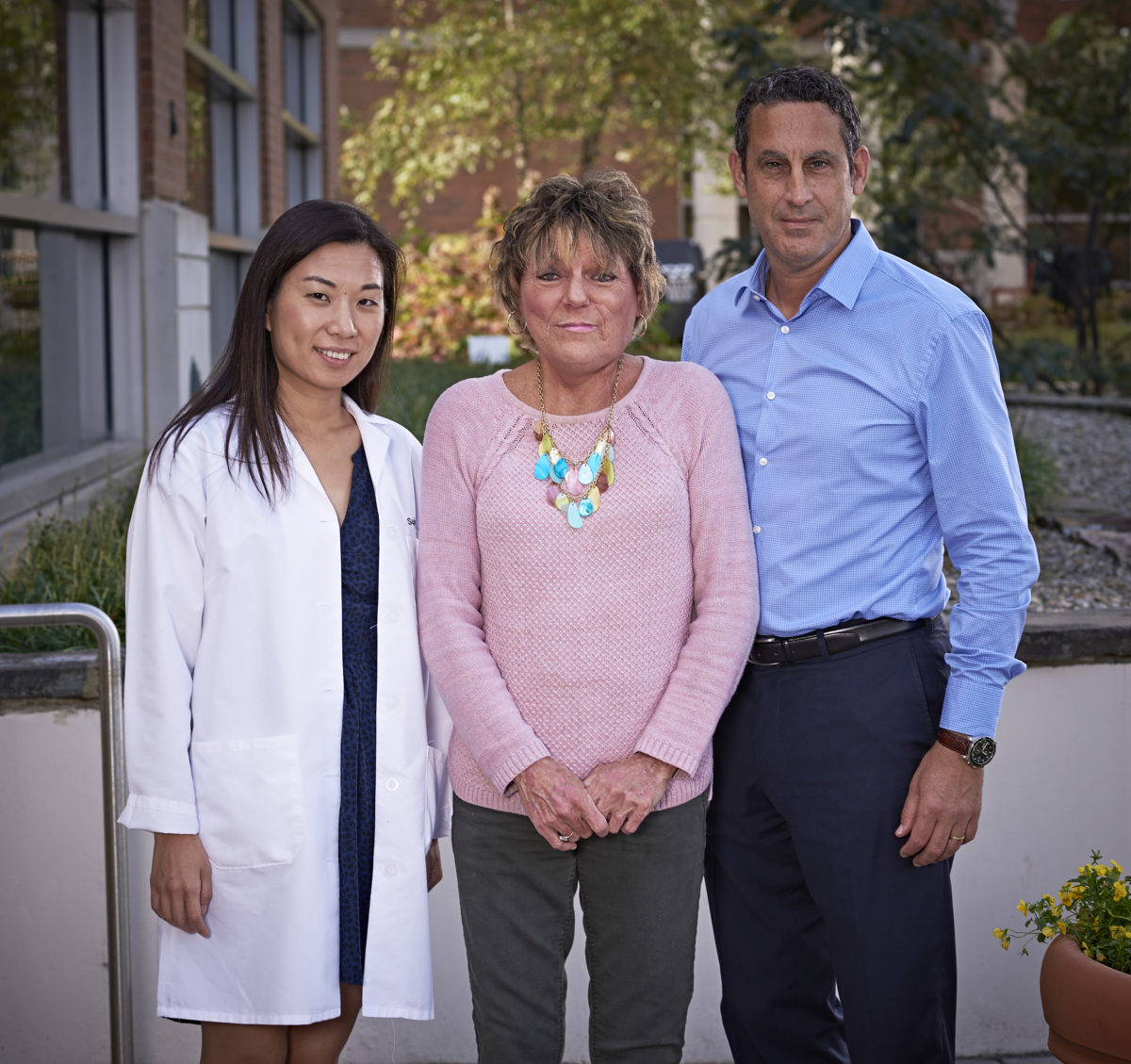
When Gloria Jeffery met with her radiation oncologist to discuss her treatment plan, she knew right away she was in good hands. Following a course of chemotherapy to shrink an aggressive oral cancer, she sat down with Adam Raben, M.D., chair of Radiation Oncology, to map out options for radiation therapy.
“Dr. Raben had me planned like a book,” Jeffery remembered. “He explained what to expect from radiation therapy and assured me he would have my back at every step. His positive, caring attitude helped me to feel more secure and positive about what I was facing.”
Jeffery’s treatment plan included a course of stereotactic whole-body radiation therapy (SBRT) followed by immunotherapy to stir up her own natural defenses to attack the cancer.
Recent research suggests that radiation appears to enhance the effects of immunotherapy not just on the targeted tumor cells, but in other places in the body where cancer may have spread.
“We have treated several patients like Gloria who seem to have what is called an ‘abscopal effect,’” Dr. Raben said. “This is where radiation to their tumor appears also to shrink other cancer cells outside the targeted area.
“The landscape and understanding of these important interactions is changing rapidly. At the second annual Immunotherapy-Radiotherapy meeting in New York City recently, I was amazed by the data presented across many malignancies and the emergence of genomic and biomarker information that shows promise in predicting response to this combination of therapies.”
Dr. Raben is leading a team of investigators in collaboration with universities and biopharmaceutical companies in an unprecedented Phase II clinical trial that combines immunotherapy and radiation after surgery for patients who have oropharynx — mouth and throat — cancers caused by the human papillomavirus (HPV). HPV-positive mouth and throat cancers are on the rise in the U.S., accelerating the drive for new clinical studies and treatments.
“We are looking to investigate and subsequently provide the least toxic therapies for people with head and neck cancer with maximum therapeutic benefit,” Dr. Raben said. “This will be the first adjuvant HPV head and neck trial in the country incorporating immunotherapy with lower doses of radiation and no chemotherapy. If successful, the trial will be a landmark for adjuvant therapy across the country. ”
The team is also working with Senior Research Scientist and Immunologist Jennifer Sims-Mourtada, Ph.D., at the Center for Translational Cancer Research at the Graham Cancer Center on pre-clinical studies to improve responses to immunotherapy. In partnership with Thomas Jefferson University, Dr. Sims-Mourtada will lead in developing and testing a new form of radiation treatment called Spatially Optimized Radiation Therapy (SORT).
Modeled on the concept of GRID-based radiotherapy, SORT will deliver tailored doses of radiation to the tumor — high doses to areas that stimulate the immune response and lower doses to areas that preserve the body’s T-cells to fight against the cancer.
The U.S. Department of Defense has invited the team to apply for a two-year, $400,000 grant to conduct a similar study of benefit to veterans, many of whom suffer from head and neck cancers that often have poor outcomes.
“Within Radiation Oncology, a primary goal is to continue to improve both inpatient and outpatient care in line with the Graham Cancer Center’s multidisciplinary model,” Dr. Raben said. “This includes participating in and initiating clinical studies that look at ways to provide the most effective and least toxic therapies for our patients.”
Patients are the heart of our team
The Radiation Oncology team collaborates in the Graham Cancer Center’s multidisciplinary approach to treating a wide range of cancers: breast, brain, gastrointestinal, gynecological, head and neck, lung, spine, prostate cancer and others. Radiation oncologists, nurses, physics and dosimetry staff, radiation therapists and clinic personnel all play an important role to ensure accurate delivery of all aspects of the radiation treatment prescription.
Following her initial diagnosis, Jeffries had come to the Graham Cancer Center to meet with doctors and nurses at the Head and Neck Multidisciplinary Center.
There she received life-saving care from Dr. Raben, as well as medical oncologists Charles J. Schneider, M.D., FACP, and SuJung Park, M.D., and head and neck surgeon Neil G. Hockstein, M.D., along with an entire team of health professionals. The team closely collaborates on care and research that often combines medical oncology and radiation therapy with surgery.
That meeting was a vital first step along a continuum of personalized care and treatment that has helped Jeffries meet the challenges of a very difficult to treat tonsil cancer that quickly spread beyond her face and neck.
“My son urged me to go to Philadelphia for a second opinion,” Jeffries recalled. “I went, but I knew I would get better care closer to home. The Radiation Oncology staff at the Graham Cancer Center feels like family to me. Everyone is so wonderful and caring, and Dr. Raben is always close by to put a smile on my face when he comes in the room.”
Leading the way to better standards of care
On any given day, some 100 patients visit the Radiation Oncology Program at the Helen F. Graham Cancer Center & Research Institute for world-class multidisciplinary care, the latest treatments and research clinical trials. The program is one of only a handful of community cancer centers to start accredited clinical residency programs to train the next generation of radiation oncologists and medical physicists.
The Radiation Oncology team not only leads the way in adapting new technologies to advance patient care, they help write the standards for best practices in care delivery. They also teach other doctors and health care professionals in their specialty.
“We are changing the platform for how we deliver radiation therapy,” said Firas Mourtada, MSE, Ph.D., D.ABR, chief of clinical physics at the Graham Cancer Center.
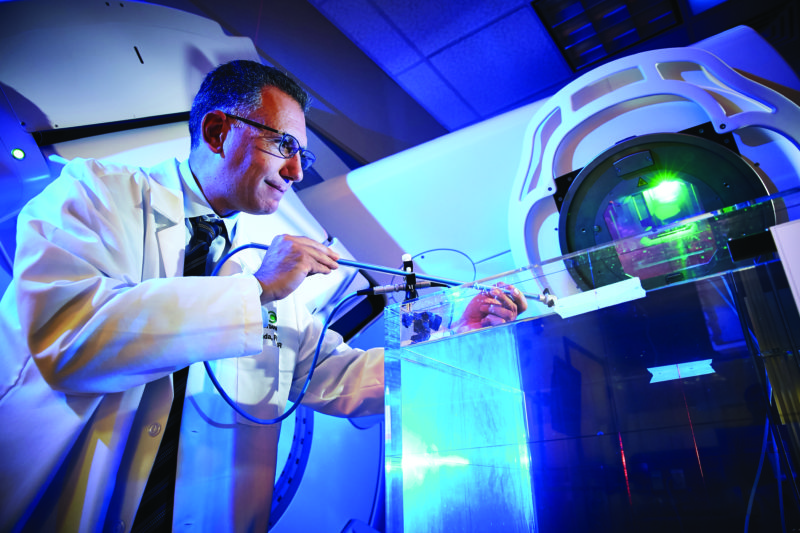
Dr. Mourtada oversees delivery of radiation treatments, working closely with radiation oncologists, physicists and dosimetrists to ensure safe and effective treatments. He is also responsible for integrating cutting-edge radiation technologies.
These include the department’s newest-generation linear accelerators that deliver external beam radiation using 4D adaptive software and the latest RayStation treatment planning to adjust and control for anatomical changes that occur in tumors and surrounding tissue during treatment. VMAT (volumetric modulated arc therapy) is now the standard of practice to dramatically reduce treatment times and optimize radiation doses to precisely target cancer cells.
Radiation Oncology offers Delaware’s first and only CyberKnife robotic radiosurgery system that targets hard-to-treat tumors particularly in the brain, lung and spinal cord, with pinpoint accuracy. Along with Cyberknife and external beam technology, there is highly conformal high-dose-rate (HDR) brachytherapy for gynecological, breast and skin cancers as well as low-dose-rate (LDR) seed implants for prostate cancer.
The team plans to add SpaceOAR hydrogels to help protect the rectum during prostate cancer radiation therapy. The biodegradable hydrogel spacers are injected into place and remain for the duration of treatment, eventually dissolving into the patient’s urine and leaving nothing behind.
Also, the latest MRI (magnetic resonance imaging) technology will be used to enhance treatment planning and post-treatment assessment for prostate and gynecological cancers. Only about 35 percent of centers around the country have incorporated MRI into their Radiation Oncology imaging toolbox.
“MRI has recently demonstrated a tremendous benefit to better delineate tumor and critical organs, in particular for cervical and prostate cancers,” Dr. Mourtada said.
“Multi-parametric MRI technology provides much higher anatomical resolution and can tell us more about the signature of the tumor than traditional ultrasound or CT or PET scans. We continue to need more advanced imaging techniques to be able to lower toxicity and protect surrounding tissues when delivering high dose radiation to prostate or gynecological tumors.”
As a board member of the American Brachytherapy Society (ABS), Dr. Mourtada helped curate a special issue of their journal featuring 12 papers from international experts on the present and future uses of MRI for the management of prostate cancer with brachytherapy. Dr Mourtada also chairs a task force for the American Association of Physicists in Medicine, charged over the next two years with writing national standards for MRI with brachytherapy.
“To advance technology in our field, we also have to train better,” Dr. Mourtada said.
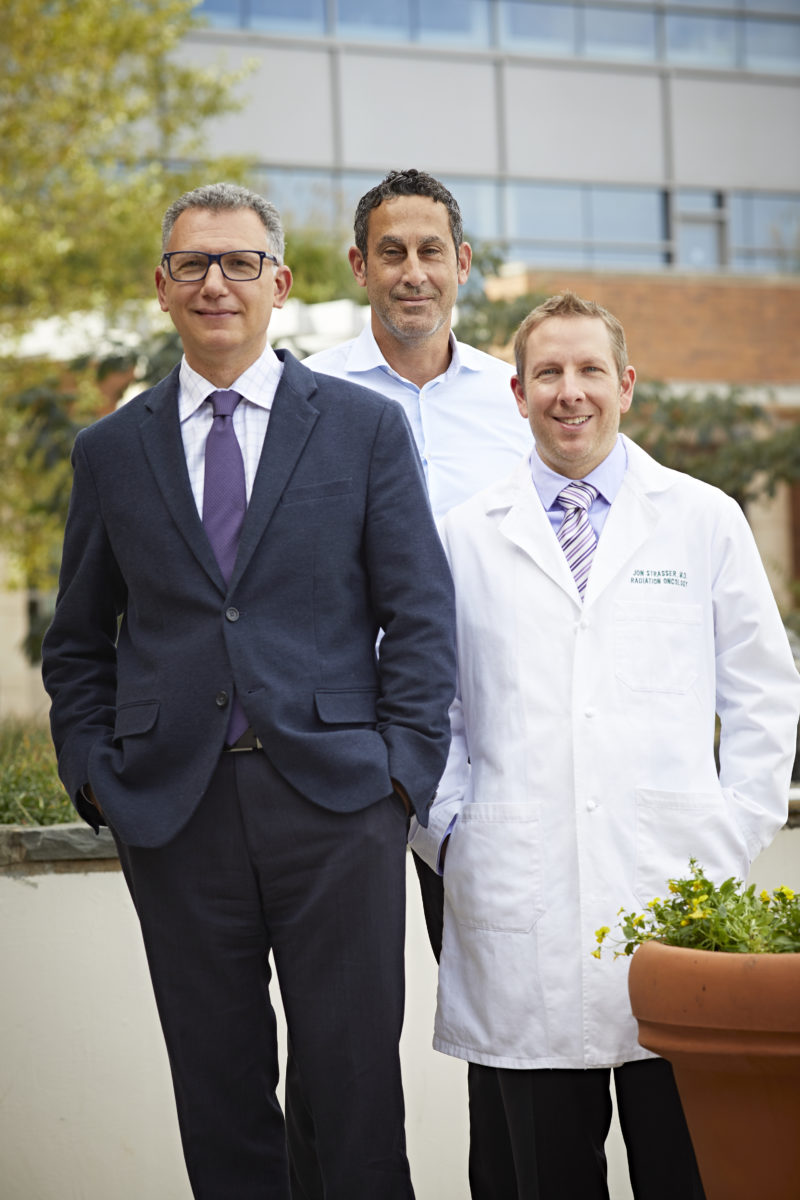
Last year, he and Dr. Raben were joined by staff medical physicist Avi Sarkar, MS, on the faculty of the ABS Prostate LDR/HDR Scholarship Education and Simulation Training Workshop in Chicago. Dr. Raben, a nationally recognized expert, led the group, using a simulated prostate model to teach advanced brachytherapy to teams of radiation oncology professionals from the U.S. and abroad.
In addition to providing continuing educational training, the department welcomes medical students and residents who rotate through from other institutions and also offers two collaborative, in-house residency-training programs. The radiation oncology physics residency program under Dr. Mourtada’s direction, offered in partnership with Thomas Jefferson University in Philadelphia, is one of only a few Spoke-Hub accredited programs in the country, accredited by the Commission on Accreditation of Medical Physics Education Programs. Now in its fifth year, the program receives more than 140 applications from top graduate programs across the U.S. to fill two highly sought-after slots. A radiation oncology residency program in partnership with Drexel University College of Medicine and Hahnemann University Hospital in Philadelphia is under the direction of Education Chief Jon Strasser, M.D.
“In-house residency programs are essential to a high-quality, forward-thinking Radiation Oncology service,” said Dr. Mourtada. “As a teaching institution, we are pushed to maintain our skill set and our technology to current standards, and collaboration with our partnering hospitals and graduate medical schools enriches our knowledge base as we strive to remain competitive.”
Radiation Oncology offices are located in the East Pavilion of the Graham Cancer Center and at Christiana Care’s Concord Health Center on Route 202 N. For information or referrals, call 302-623-4800.