Ruptured aneurysms and strokes don’t only impact individuals. They change the dynamic of an entire family, potentially for generations to come.
Christina Moore was 34 in 2014, when she suddenly suffered a thunderclap headache. She and her husband Leonard had come from their home in Bel Air, Maryland, to a friend’s birthday party in Bear.
“The pain and nausea were so intense, I knew it was something really bad,” she said.
Leonard, a former Christiana Care employee, recognized something was terribly wrong. He insisted his wife be immediately transported to Christiana Hospital, which today is the only Joint Commission designated comprehensive stroke center in the region outside of the urban centers in Baltimore and Philadelphia. Comprehensive stroke centers are able to provide the most advanced level of expertise in stroke care.
“He said Christiana Hospital was where I needed to be,” she said.

In the Emergency Department, CT scans of Christina’s head revealed that she had suffered a ruptured “blister” brain aneurysm, a rare and difficult-to-treat condition.
“It was a very unusual case because she never smoked and she is young, with no family history of aneurysms,” said Sudhakar Satti, M.D., the neurointerventional surgeon who treated her. “Her only risk factor for this rare subtype of brain aneurysm was being a woman of Asian descent.”
Patients who survive these ruptured aneurysms often have severe permanent deficits that devastate the dynamics of an entire family.
“They go from being the person who takes care of the family to someone who requires constant care,” Dr. Satti said.
Christina was initially treated with coiling, a minimally invasive endovascular procedure. But her condition continued to deteriorate. She experienced extreme cerebral vasospasm, a narrowing of blood vessels of the brain that reduces blood flow and causes delayed ischemic strokes.
“The Neurointerventional Surgery team had to take her back to the interventional suite multiple times to treat these spasms despite maximal medical therapy to prevent her from suffering a stroke,” Dr. Satti said.

Despite the initial coiling procedure, her aneurysm recurred in one week. After a multidisciplinary review of her case, it was determined that Christina would be best served with a novel flexible, flow-diverting intracranial stent. This stent diverts flow from the aneurysm, and allows the aneurysm to clot and ultimately shrink while allowing the patient’s own vessel to heal itself.
Once the healing is complete, the aneurysm is permanently cured without need for additional surgery or follow-up.
“Cases like these highlight the importance of a team-driven approach to complex cerebrovascular patients that leverages the combined expertise of neuroscience specialties, including neurosurgery, neurocritical care, stroke neurology and neurointerventional surgery,” he said.
Christina’s condition was stable, but she was still extremely ill and spent several weeks in the Neurocritical Care Unit. Eventually, she was well enough to go to a rehabilitation center. But her struggle continued.
“I had to learn to walk all over again,” she said. “I thank God and the people who took care of me for getting me through.”
Back home in Maryland, Christina continued to reclaim her life. She and her husband wanted to have a baby, but her obstetrician was concerned that her medical history would put her at risk.
Dr. Satti performed a follow-up transradial cerebral angiogram that confirmed complete aneurysm healing. She was cleared from any physical restrictions, including pregnancy.
“The aneurysm was completely gone. The native vessel is healed, and the aneurysm should never recur,” Dr. Satti said.
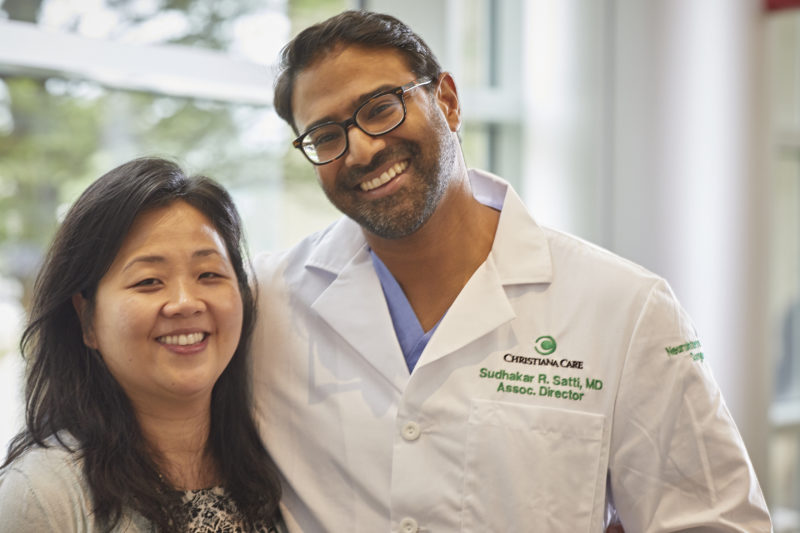
In 2016, two years later, Christina and Leonard welcomed Apollo, a healthy boy, into the world. Dr. Satti consulted with her obstetrician and visited mom and baby in the hospital.
“These kinds of outcomes have a ripple effect,” he said. “Christina went from being very sick to getting well and bringing the next generation into the world.”
For her care team at Christiana Care, Christina’s recovery and her ability to start a family is a joyful reminder of the value and importance of the work they do every day.
“This is a great example of a team-based approach across specialties, driven by the service line model and the positive impact we can have on patient care when we serve together to deliver on the Christiana Care Way,” said Valerie Dechant, M.D., clinical leader of Neurosciences and medical director of Neurocritical Care and Acute Neurologic Services.



