At Christiana Care, patients are at the center of care. That is why patient and family advisers play a key role in meeting the challenges of sweeping changes in health care, said Janice E. Nevin, M.D., MPH, president and CEO.
Dr. Nevin spoke at the quarterly meeting of the Patient and Family Advisory Council on Oct. 7. She said the insights of volunteer advisers are essential to the collaborative process that will help the health system achieve its goals of optimal health, exceptional experience and organizational vitality.
“You have shown us that to be healed is more than just great medical care,” Dr. Nevin said.
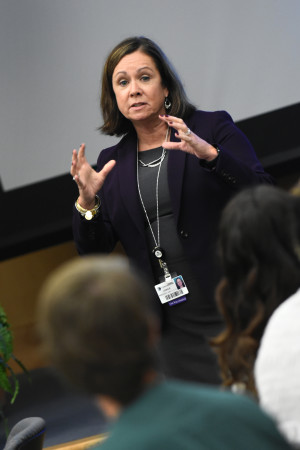
She recalled that when the Intensive Care Unit at Wilmington Hospital was relocated, patient advisers were on-site at 5 a.m. to help with the transition.
“These volunteers demonstrate an extraordinary commitment to patients and staff,” she said. “You have transformed us as an organization.”
The number of patient and family advisers at Christiana Care has grown significantly over the last two years, with groups at both Wilmington Hospital and Christiana Hospital. Currently more than 100 patient and family advisers and more than 40 staff advisers help to guide Christiana Care.
“When we ask for volunteers and input, the teams are quick to respond and engage with us in adding value to our care,” said Ann-Marie Baker, MSN, RN BC, senior program manager, Patient Experience, and coordinator of patient and family advisory work.
Advisers provide viewpoints that can dramatically change a project, a product and outcomes. The quarterly meeting itself was designed with feedback from advisers who wanted to bring the entire group of advisers together to collaborate on larger systemwide projects.
“We have built a community within our patient and family advisers that provides value to Christiana Care, to the many people we serve, and to these individuals who so generously volunteer their time and hard work,” said Shawn R. Smith, MBA, vice president, Patient Experience.
The advisers focused on two important projects during the meeting: redesigning patient gowns and enhancing the patient discharge process.
“This is so rewarding,” Smith said. “The excitement and enthusiasm of these advisers is contagious, knowing that these two unique projects have the potential to impact every single patient we serve.”

Three prototypes of gowns, designed in collaboration with the University of Delaware, were passed around the auditorium at the John Ammon Medical Education Center so advisers could scrutinize the fabric and construction. Many tried them on for size.
“We’re looking for ways the patient can be covered up while still allowing the caregiver to have access to the patient,” said Renee Tomczak, patient adviser.
They learned that designing a simple gown is a complex proposition. Can it accommodate a nursing mother? Can leads for monitoring the patient be readily passed through the pocket? Can the gown be easily removed when a patient has surgery? Is there a better way to secure the gown than the ties currently in use?
The advisers learned that plastic snaps can be warped by the high heat in the hospital laundry. Velcro soon picks up lint and its edges grow sharp, which could harm patients’ skin. Metal snaps are durable, but are they easy for patients to manage?
Advisers will continue to provide input after the gowns are tested in several patient care units. The group also evaluated a questionnaire designed to make the discharge process more patient-friendly.
Advisers appreciated the concept of providing a list of tips and questions that patients and families can readily reference. They suggested streamlining the list or developing two separate sets of tips, with one list focusing on the day of discharge.
“Being in the hospital can be overwhelming,” Tomczak said. “We don’t want to overload patients.”



















































