Simulation training sharpens clinical skills and understanding
A dozen members of a multidisciplinary stroke team, with representatives from the Emergency Department, neurointensive care, Heart & Vascular Interventional Services (HVIS), neurointerventional surgery and anesthesia, gathered in the Virtual Education and Training Simulation (VEST) Center at Christiana Care on a recent morning.
6,893 practitioners from a wide range of medical disciplines trained at the VEST Center last year.
They were there to run through procedures with a goal of standardizing the response to acute stroke patients that arrive in HVIS for acute intervention. And to begin, Laura Giannini, RN, nurse in the Emergency Department, wheeled in a stretcher with a patient simulator named Vera Miller.
A 62-year-woman with hypertension, asthma and a touch of arthritis, Vera, a robotic mannequin, arrived with a specific scenario: She had fallen at the start of her day and was unable to speak or move her right side. Giannini told the intervention team that Vera scored 21 on the standardized stroke scale of the National Institutes of Health, which indicated a severe stroke.
Then the team of HVIS nurses and technicians, as well as the anesthesia team, physically and verbally ran through the procedures they would perform on a patient like Vera. As they did, Barbara J. Albani, M.D., medical director of neuroInterventional surgery, watched intently from the next room.

Dr. Albani is seeking ways for the team to standardize the process of prepping the patient for intervention in an effort to minimize the time from when the patient arrives at the HVIS door to the time of incision. The goal is to consistently reduce that time to 20 minutes or less.
“With acute stroke we say ‘time is brain,’” said Dr. Albani. “There is no more sensitive organ to the loss of oxygen than the brain. There are so many roadblocks that are placed in our way when trying to restore blood flow to the brain that we cannot control, like how long it takes the patient to present to the hospital. What we are trying to do is minimize a segment of time where we do have control. Getting providers comfortable with the process of an HVIS stroke code will minimize wasted time, because everyone will know what to do, decreasing redundancy. The faster we get the blood vessels open, the better patients do in the long run. When we are working efficiently, we can take a patient who arrives to us neurologically devastated and make a profound impact on their functional recovery.”

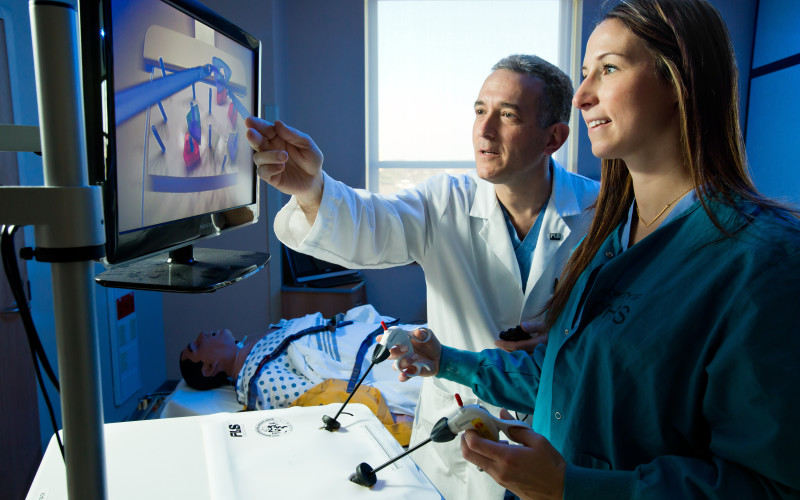
Team leaders at Christiana Care often want to run through this type of scenario, then step back and assess what they have observed, as they move toward a best-practice model, said Susan Coffey Zern, M.D., CHSE, director of simulation. According to the Society for Simulation in Healthcare, simulation can accommodate a range of learners, from novices to experts. Beginners gain confidence and muscle memory from practice drills, leading to greater expertise. And through simulation, well-trained practitioners can master the growing array of new technologies, such as minimally invasive surgery and catheter-based therapies, without putting patients at risk.

For all these reasons, the use of simulation is expanding at Christiana Care and around the nation. In November, a second simulation center opened on the 8th floor of Wilmington Hospital in a spacious suite that has two high-fidelity mannequins and many simulation programs. A goal is to make the new simulation center a hub of training for family practice, minimally invasive surgery training for general surgery residents, as well as oral and maxillofacial surgery, and anyone else interested in learning, said Dr. Coffey Zern. All are departments based at Wilmington hospital.
The first Virtual Education and Simulation Training Center in the John H. Ammon Medical Education Center opened in 2009. In the last academic year, 6,893 people trained in the center. “People repeatedly see that simulation is wonderful for performance improvement,” said Dr. Coffey Zern.
For example, simulation training was recently expanded for speech pathologists learning to perform fiberoptic endoscopic evaluation of swallowing (FEES), a procedure that involves passing an endoscope transnasally to the hypopharynx of a patient to assess swallowing function. The project, which won a Focus on Excellence Award, demonstrated that simulation training paired with traditional training methods improved the timeliness and scoping accuracy with which the trainees were able to perform the procedure.
“Simulation training brought our FEES program to a new level of excellence,” said Dale R. Gregore, MS, CCC SLP, BCS-S, program manager, Speech Pathology. “Not only did clinician decision-making improve during realtime scenarios, such as change in vitals, but clinician confidence increased. As a result, overall FEES competency was attained in six to nine months, versus more than a year using traditional teaching methods alone.”
Simulation training has been a powerful tool in building skills among surgeons using the da Vinci Robotic Surgery System. The da Vinci system enables surgeons to perform delicate procedures through very small incisions with great precision, and training on the robotic system is important for even experienced laparoscopic surgeons who wish to use robotics.
A committee of surgeons set up standards for training on the da Vinci system, requiring two scores of 90 percent proficiency ratings on a series of 10 dexterity drills. A study of posttraining performance showed that real-world results were outstanding for eight surgeons who met the training requirements.
“No one would go into a major league game without first taking batting practice and making sure they are in the groove,” said Jeffry Zern, M.D., head of minimally invasive surgery. “As surgeons, we can only expect to be in the groove when we have a chance to practice, too.”