Meet Nancy Kirby, manager of Occupational Safety, who extols the rapid response of her team to the early requirement for thousands of caregivers to be fitted for new N95 respirators and other urgent needs.
Q. How has your typical workday changed? What work are you doing that’s new or different because of COVID-19?
A. Early on we had to adjust to a large increase in the scale of one of our major jobs. Most people by now have heard about the role of N95 respirators as a crucial piece of personal protective equipment in the fight to prevent spread of COVID-19 infection, and might even know a bit about them – like when they’re needed, how they are donned and doffed, and especially, their current availability or lack of it.

At ChristianaCare the N95 was a common safety tool even before the pandemic arrived and it has been the responsibility of ChristianaCare’s Occupational Safety team to ensure that they fit our caregivers so that they function as expected. Our job is to make sure the respirator seals around the face so no contaminants get inside.
Previously,N95s were primarily for protecting staff who work with tuberculosis patients. But due to the rapid rise of COVID-19 infections the team had to react quickly when our supply of the respirators started to diminish.
We began to rely on the state of Delaware’s stockpile of the masks, which were a different design, requiring everyone who potentially would need a mask to be retested. So we fit-tested 3,007 caregivers between March 13 through April 17. That amounts to more fit testing than in all of 2018, when 2,765 caregiver fittings occurred. In 2019 her team fit-tested 2,496.
Q. What is fit testing?
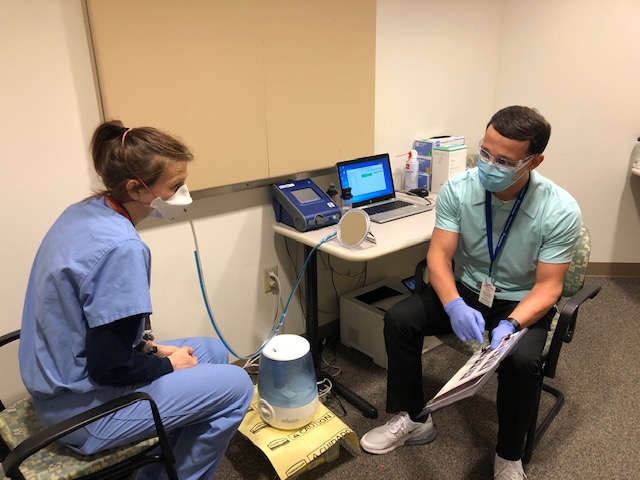
Fit testing is a pass/fail process that evaluates the seal of the respirator to the face. It’s an annual OSHA requirement. With just one technician to do the fit tests we were going full tilt in the first couple weeks of the pandemic. There are three machines that can be used for the tests, so we reassigned a lot of our staff in the department to do the job in a big rush. We also utilized redeployed caregivers, which was extremely helpful. At one point the testing was going 20 hours a day at both hospitals, 6 a.m. to 2 a.m.
Q. Why were so many tests required in such a short span of time?
A. As the pandemic continued, ChristianaCare’s supply of N95s began to diminish and shipments from our suppliers could not be increased. The State of Delaware maintained a stockpile to support hospitals in the event of an emergency. Since the State model was different than the model being used by ChristianaCare, all caregivers using the State model had to be fit tested on that model per OSHA regulations.
Now that the pace of fit testing is lessened Occupational Safety has begun reviewing donated N95s and alternative respirators to determine which ones can be used at ChristianaCare. For example, New Castle County Vo-Tech School District donated several thousand N95s. Other sources, such as construction companies, have also contributed, and we’ve been vetting those masks for possible use in health care.
Q. What happens if a caregiver fails a fit test?
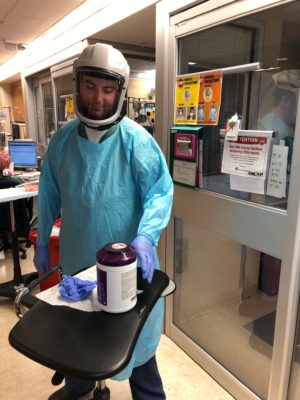
A. For various reasons, not everyone can be fitted for the N95, but may still require protection. In that case, the caregiver can be issued a powered air purifying respirator (PAPR). Commonly, PAPRs come with a disposable hood, which were becoming hard to get. Occupational Safety was able to obtain reusable helmet-type headgear for the PAPRs, which were very well received by caregivers using them.