For the first time in Delaware, and likely the nation, cancer specialists have co-authored a consensus statement and clinical pathway for the management of colon cancer that has spread to the peritoneum or abdominal wall. The statement has been published in the Jan. 10 online issue of Surgical Oncology.
The statement aligns the state’s major health care providers on a standardized, evidence-based approach to the treatment of this kind of colon cancer. This will ensure patients throughout the state will receive optimal care and equitable access to the most appropriate treatment options and clinical trials.
Medical and surgical oncologists from ChristianaCare’s Helen F. Graham Cancer Center & Research Institute, Tunnell Cancer Center at Beebe Healthcare and TidalHealth Allen Cancer Center prepared the statement “Consensus Statement and Clinical Pathway for the Management of Colon Cancer With Peritoneal Metastases in the State of Delaware.”
The statement was published on behalf of the State of Delaware Peritoneal Surface Malignancies Task Force.
Close to home for cancer care
“Consensus among cancer specialists on how to treat colon cancer patients with peritoneal malignancy will assure that these patients have access to the specialized treatment they need at an experienced cancer center right here in Delaware,” said co-author Nicholas Petrelli, M.D., Bank of America endowed medical director of the Helen F. Graham Cancer Center & Research Institute.
To schedule an appointment at the Helen F. Graham Cancer Center & Research Institute, call 302-623-4500.
“As cancer care providers, we know how important it is for patients to be close to home for their cancer care.”
“Getting cancer physicians throughout the state to agree on who is eligible for treatment and the right sequence of therapies was no small task,” said lead author Jesus Esquivel, M.D., co-director of Beebe Healthcare’s Peritoneal Surface Malignancy Program.
“Thanks to Dr. Petrelli’s leadership, coupled with the support of a very committed task force, we have been able to make this happen on a statewide level.”
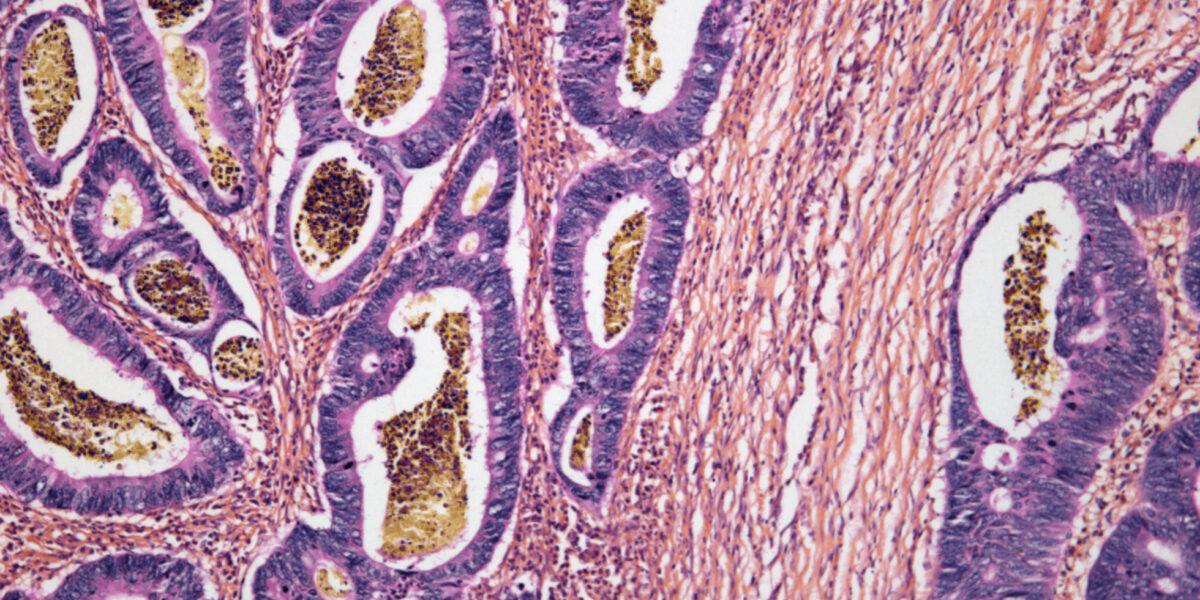
In about 10% to 20% of cases, colon cancer is found in the peritoneum, the lining of the abdomen that covers the abdominal organs. Historically, patients with peritoneal metastases have a worse prognosis. However, numerous studies show five-year survival rates for patients whose peritoneal cancer can be surgically removed approach the rates of those with successful surgery for metastatic liver disease.
“We are looking at a complicated group of patients with advanced colon cancer and a generally poor prognosis, who historically have been treated in a non-uniform fashion despite medical evidence to suggest which therapies are most effective,” Esquivel said.
Combining surgery and heated chemotherapy
The Delaware pathway includes a combination treatment of surgery and heated chemotherapy, starting with cytoreductive surgery (CRS) to remove all visible cancer in the peritoneum. Hyperthermic Intraperitoneal Chemotherapy (HIPEC) with Mitomycin C is then delivered on the operating table for 90 minutes. Mounting clinical evidence shows this one-two punch can significantly extend survival in well-selected patients when compared with standard systemic chemotherapy.
“Patients will have access to the specialized treatment they need at an experienced cancer center right here in Delaware.”
— Nicholas Petrelli, M.D.
Currently, due to a steep learning curve, only about 120 hospitals in the U.S. have the necessary capability and expertise to perform these procedures. In Delaware, only ChristianaCare and Beebe Healthcare can offer patients CRS with HIPEC.
Some patients who are not immediate candidates for surgery may benefit from systemic therapy (chemotherapy/ immunotherapy) as a first-round treatment. Others on the pathway may be recommended for systemic therapy alone and potential participation in an appropriate clinical trial.
Four-tier scoring system
To help providers determine the best form of treatment for each individual patient, the Delaware pathway introduces the Peritoneal Surface Disease Severity Score (PSDSS). The scoring system uses four tiers of estimated disease severity based on a three-point scale that includes symptoms, extent of peritoneal dissemination and primary tumor histology.
“With the Delaware pathway in place, our goal is to ensure that multidisciplinary evaluation begins at the time of diagnosis so that each patient is selected for the right sequence of currently available therapy depending the individual cancer,” Esquivel said.
“Not only are we recommending a uniform treatment modality for patients, but our framework facilitates data reporting and evaluation that will add to the body of knowledge about this disease and how best to treat it.”
Although there is plenty of medical evidence to suggest which therapies are most effective, until now, efforts by Esquivel and others to achieve consensus worldwide have not translated into a universally accepted clinical pathway for the management of this disease.
With the Delaware pathway, multidisciplinary evaluation can begin at the time of diagnosis so each patient is selected for the right sequence of therapy.
Delaware is a unique launching pad for such a pathway.
“As cancer care providers we know how important it is to work together on behalf of our patients,” said Petrelli.
“Delaware is uniquely suited to this effort not only because of its size, but also because of the collaborative relationships we have built through groups like the Delaware Cancer Advisory Council and Consortium and most specifically for this effort, the Delaware Peritoneal Surface Malignancy Task Force.”
The Delaware Health Information Network (DHIN) is another important resource to assist physician collaboration. Nearly 100% of the state’s medical providers are linked in. The DHIN launched in 2007 as the first operating statewide health information exchange in the country.
“I don’t expect 100% of patients to be included in the pathway, but I see it as the best opportunity for patients to maximize benefits and minimize suffering or unnecessary treatment,” Esquivel said.
“As a health care provider who treats patients with advanced cancer, I know that is the best one can hope for short of a cure.
“With consensus on evidence-based clinical pathways, we can offer increasing numbers of patients the assurance that whether you live in northern or southern Delaware, you can rely on getting the best treatment available for your cancer.”