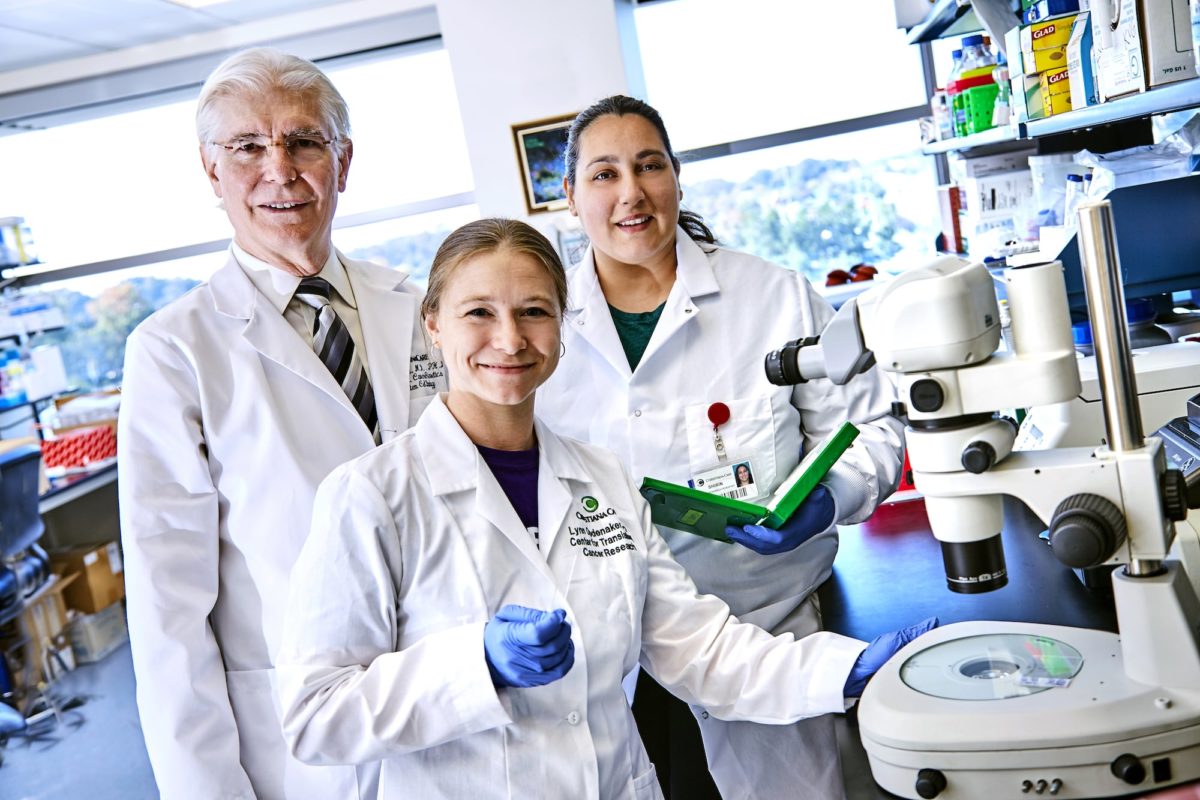
In a discovery that may have significant impact on the future of colon cancer treatment and research, scientists at the Helen F. Graham Cancer & Research Institute’s Center for Translational Cancer Research at Christiana Care Health System have defined a key signaling pathway that regulates colon cancer growth.
The study, led by Senior Research Scientist Bruce Boman, M.D., Ph.D., MSPH, FACP, is reported in the October 5 issue of Oncotarget.

“Our findings point to a number of possibilities for developing more effective stem cell targeting therapies for advanced colorectal cancer,” Dr. Boman said.
Conventional research over the last 50 years has been guided by the idea that tumors undergo a series of genetic mutations that lead to the unchecked growth of tumors and their progression to metastatic cancer. Traditional therapies designed to kill the bulk of cancer tumor cells continue to fall short of a cure for advanced, drug-resistant colon cancers.
Treat cancer by eliminating cancer stem cells
“Our thinking has shifted to the insight that cancers originate in tissue stem cells through dysregulation or malfunction of the self-renewal process, and that cancer stem cells drive tumor growth,” he said. “It follows that the optimal way to treat cancer (especially advanced cancer) is to eliminate cancer stem cells.”
Tumors develop when certain mutations or mistakes occur in the genes of normal tissue cells that regulate stem cell renewal and population size.
“We discovered that the retinoic acid or RA signaling pathway acts to induce differentiation of colon cancer stem cells and reduce cancer stem cell overpopulation, which puts the brakes on the primary mechanism that drives colon cancer development,” Dr. Boman explained.
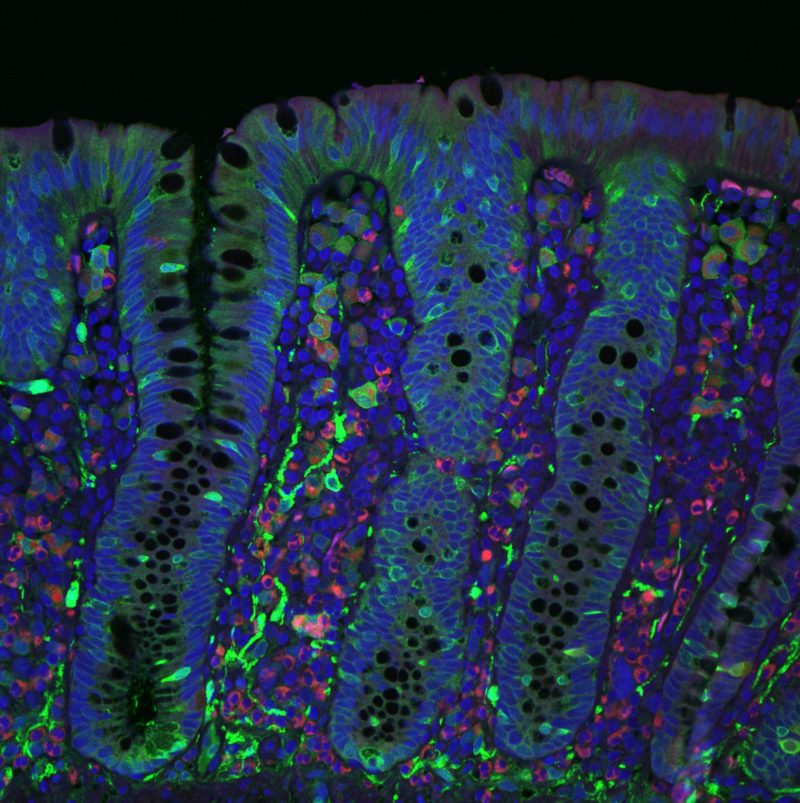
Previous studies in Dr. Boman’s lab pinpointed aldehyde dehydrogenase (ALDH) as a biomarker for normal and malignant human colon stem cells and showed that ALDH tracks stem cell overpopulation during the formation of colon tumors.
Because ALDH is both a marker for stem cells in many tissues and a key enzyme in retinoid acid signaling, Dr. Boman’s research team at the Graham Cancer Center pursued further study of the retinoid signaling pathway in normal and malignant colonic stem cells.
What they found is that the anti-cancer effects of retinoic acid signaling in colon cancer occurs through decreased growth of ALDH-positive colon cancer stem cells – the cells that carry the ALDH marker.
Retinoic acid also increases differentiation of cancer stem cells, which decreases their self-renewal ability and inhibits cell proliferation. Differentiation is where unspecialized stem cells acquire cellular traits that allow them to perform specialized functions, such as uptake of water and nutrients, for example.
Based on these findings, the investigators concluded that retinoic acid signaling provides a mechanism to selectively target colon cancer stem cells and reduce the self-renewal ability of those stem cells during cancer development.
Their findings suggest treatment with retinoid drugs, which are derived from vitamin A, could provide a therapeutic strategy to selectively target cancer stem cells and decrease the number of highly resistant cancer cells.
To test this possibility, they chose all-trans retinoic acid (ATRA), one of the most commonly investigated and clinically tested retinoic acid derivatives. Previous studies have shown that ATRA can reduce self-renewal ability in a number of other cancers.
The investigators found that ATRA down-regulates gene expression of the ALDH stem cell biomarker and reduces stem cell viability and renewal, and therefore abates tumor growth.
“Dr. Boman presents us with a broader view into the origins of colorectal cancer at the cellular and molecular level,” said Nicholas J. Petrelli, M.D., Bank of America endowed medical director of Christiana Care’s Helen F. Graham Cancer Center & Research Institute.
“His work highlights the mission of the Center for Translational Cancer Research to hasten discoveries from bench to bedside and draws us even closer on the path to targeted therapies that can improve survival and quality of life for patients with drug-resistant, advanced colorectal cancer,” Dr. Petrelli said
Colorectal cancer is the second leading cause of cancer-related deaths in the United States, equally affecting both men and women.
The lead author on the paper, titled, “The anti-cancer effect of retinoic acid signaling in CRC occurs via decreased growth of ALDH+ colon cancer stem cells and increased differentiation of stem cells” is former University of Delaware student researcher Shirin Modarai, Ph.D., who is now a research scientist at the Helen F. Graham Cancer Center & Research Institute.
Co-authors who worked on the project while at Christiana Care are Lynn Opdenaker, Ph.D., Anindita Gupta, MS, Ryan Kowash, Gabriel Masters, Vignesh Viswanathan, Ph.D., and Tao Zhang, M.D., Ph.D., as well as Jeremy Z. Fields, Ph.D. of CA-TX Inc., Princeton, New Jersey.
The study was funded in part by the National Institutes of Health (Grant number: P20RR-1 6472-04) and the Cancer *B* Ware Foundation.