Sickle cell disease is one of the most common inherited blood disorders in the Black population. It also affects people of Latino and Middle Eastern descent. Although acute and chronic pain are common with sickle cell disease, patients may feel hesitant to seek treatment.

“Pain is the most common complication, yet pain can be underreported by patients or misunderstood by health care providers as opioid-seeking,” said Stephanie Guarino, M.D., MSHP, clinical lead for the Sickle Cell Program at ChristianaCare’s Center for Special Health Care Needs, which provides primary care for adults with complex conditions that start in childhood. It is the only Delaware-area center of its kind.
Patients and health care providers wishing to learn about the study may call the Sickle Cell Program at the Center for Special Health Care Needs at 302-320-6300, option 5.
“One of the misconceptions is that people with sickle cell disease are just seeking pain medications,” said Dr. Guarino, who is also a pediatric hematologist and oncologist at Nemours Children’s Health, home to the Delaware Comprehensive Sickle Cell Research Center.
“But we’ve found that people are much more interested in other non-medication ways to manage pain.”
To help these patients, Dr. Guarino is the lead on a ChristianaCare-based study that will determine if peer-led support groups can offer pain-relief strategies and help participants overcome stigma.
A lifelong disease
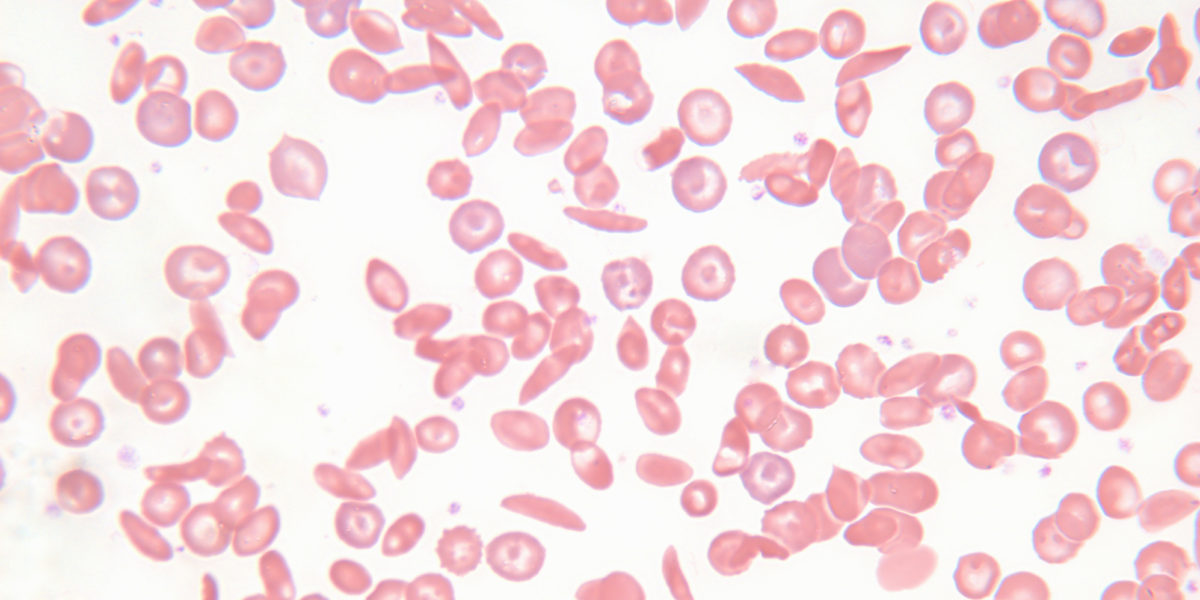
Sickle cell disease is aptly named. Healthy red blood cells are round and flexible. In people with sickle cell disease, the red blood cells can form half-moon or “sickle” shapes. The stiff cells can stick to each other and cling to blood vessel walls. When a buildup inhibits blood flow, organs and tissue don’t receive adequate oxygen. Patients can experience eye problems, swelling in the hands and feet, strokes, joint issues and leg ulcers.
Because the disease spans a lifetime, it requires a continuum of care. The Delaware Comprehensive Sickle Cell Research Center, one of the National Institutes of Health Centers of Biomedical Research Excellence (COBRE), was created to meet patients’ ongoing needs. ChristianaCare is a partner.
The center recently received a $10.5 million COBRE grant that will fund four projects, including the research led by Dr. Guarino at ChristianaCare. The current project is an extension of her 2019 pain-management survey, which found that respondents received massages, took baths and listened to music to combat discomfort, often trying these techniques before or instead of medication.
“More than 80% recognized the connection between stress level and pain,” she said. Emotion also plays a part, she said.
Taking the next step
Using the curriculum from the ChristianaCare Comprehensive Pain Center, Dr. Guarino and her team gathered patient feedback to make the content more relevant to sickle cell disease and address racism and stigma attached to care.
“Every step of the way, we are getting advice from patients with sickle cell disease, families and caregivers.”
Dr. Stephanie Guarino
Now the researchers will take the sickle cell disease-specific curriculum back to patients and families and pilot a peer-led group.
“People with sickle cell disease want to hear from others with sickle cell disease,” she said. “We are looking to show that peers can be trained to be effective moderators for group interventions.”
The sessions will take place in the hospital, at a neutral off-site location or virtually.
“Every step of the way, we are getting advice from patients with sickle cell disease, families and caregivers,” she said.
“We’re incredibly excited to be able to address some of the disparities and improve the care for people with sickle cell disease,” Dr. Guarino said.
The research team also includes Lee Pacher, D.O., a senior physician scientist at ChristianaCare; Keshab Subedi, MS, MSC, a ChristianaCare biostatistician in the Biostatistics Epidemiology Research Design (BERD) core of Delaware ACCEL-Center for Translational Research; Mia Papas, Ph.D., MS, corporate director of the ChristianaCare’s Institute for Research on Equity and Community (iREACH); Charmaine Wright, M.D., MSHP, medical director of ChristianaCare’s Center for Special Needs; Olu Bakare, M.D., MPH, sickle cell research coordinator in the Center for Special Health Care Needs; and Claudine Jurkovitz, M.D., MPH, senior physician-scientist in the ChristianaCare iREACH.
Click here to learn more about sickle cell disease.