From Acute Medicine to Women’s and Children’s, the service lines and essential services of Christiana Care Health System are sharing success stories from their first year of implementing clinical pathways as they roll out the second set of these medical road maps, designed to reduce unnecessary variation in care, improve patients’ health and experience, and reduce health care costs.
The new pathways range from providing early supportive care for about 100 cancer patients undergoing multiple modes of treatment to optimizing the health of all who are preparing for surgery.

“This process has exceeded my expectations, the way teams have come together on this work,” said Ken Silverstein, M.D., MBA, chief clinical officer. “What’s special is we’re improving outcomes. We’re reducing things like readmissions. All of our patients have been touched, because the entire clinical system has been focused on this.”
Clinical pathways enable doctors, nurses and other care providers to implement standardized but individualized plans of care informed by the most up-to-date information. They include algorithms for screening, evaluation, diagnosis and treatment, answers to common questions or concerns, recommendations for patient-education materials, information about resources available to patients and their families, and recommendations for follow-up and preventive care.
One of the keys to the pathways’ success is that they standardize protocols, ensuring that all patients receive the right care, at the right time, with the right team involved, 100 percent of the time.
“There are places where variation is appropriate, but unnecessary variation does not provide an environment for the patient to have the best health outcome, and there are costs related to that,” Dr. Silverstein said.
The approach is breaking down traditionally siloed areas of the health system, creating robust collaboration among service lines and essential services. The process is governed by the Clinical Value Council and Clinical Value Executive Committee. A Pathway Integration Team supports systemwide implementation, and a Project Manager Forum supports the integrated practice teams (IPTs) tasked with developing the pathways for their service lines.
“People are excited for these new relationships,” he said.
The pathways aren’t static documents. They are ever-evolving, guided by new research and experience, always with the potential to support coordinated leaps forward in delivering optimal health and an exceptional experience to the people we serve. In Women’s and Children’s, for example, feedback surrounding a new testing approach for women with gestational diabetes — the service line’s inaugural clinical pathway under the new process — led the service line to regroup and create a whole new, more efficient obstetrical visit that has been embraced by patients.
“The vision is that this competency will become inherent in all that we do, and the service lines will continue to forge ahead on their own,” he said. “We’re still learning, but at some point you will see this clinical pathway development process as being self-sustaining. It’s the kind of collaboration our patients deserve.”
While the clinical pathways are currently being used primarily in Christiana Care’s hospitals and outpatient practices, they are published online at http://pathways.christianacare.org. As this library of clinical pathways grows — along with their implementation — they have the potential to support better coordinated and optimized care for patients throughout the community, as physicians and other care providers will be able to leverage the pathways throughout the continuum of care.

Acute Medicine: Lower gastrointestinal bleeding
Building on a body of research that was already under way, the Acute Medicine service line chose lower gastrointestinal bleeding for its new clinical pathway.
“The diagnosis falls within Acute Medicine, but it touches a lot of different areas — primary care physicians, the Emergency Department, surgeons, nuclear medicine,” said Kate Rudolph, M.S., administrative director of Inpatient Medicine. “There’s a lot of complexity, and it’s very, very resource-intensive. And yet, we haven’t significantly improved outcomes.”
The service line has assembled a multidisciplinary team to achieve consensus on a standardized treatment plan for the estimated 100 to 170 patients that Christiana Care Health System treats for lower GI bleed each year, Rudolph said.
“If we can have a more team-based approach across specialties, at each step of managing this condition we will be setting the patient up for the next successful step of treatment,” she said.

The team identified opportunities to improve care while reducing costs, said Virginia Collier, M.D., MACP, physician leader of the Acute Medicine service line and Hugh R. Sharp Jr. Chair of Medicine. For example, the service line found that it had been over-utilizing the RBC nuclear scan, which measures a patient’s rate of bleeding.
“If the patient is bleeding slowly, a bleeding scan will be negative,” Dr. Collier said. “Ordering the study increased the time to diagnosis and resulted in additional costs. Performing the scan did not provide value to the patient.”
The new treatment approach is expected to improve patient outcomes, shorten the length of stay, lower the cost per patient, reduce unnecessary testing and provide a better transition to outpatient services.
“We are doing our best to make this a patient-focused pathway, providing education to help patients understand their condition and be an active participant in their care,” Rudolph said.
Meanwhile, Acute Medicine is seeing success with the chronic obstructive pulmonary disease (COPD) clinical pathway that was developed last year.
Since Jan. 1, 470 patients have been enrolled in the COPD clinical pathway, which has resulted in a reduction in readmission rates below the target of 24 percent to 17.34 percent.
The service line also has improved home health utilization. Of the patients enrolled to-date, 16 are in hospice, 197 are at home with the help of a home health care organization, and 193 are living independently.
The next challenge for the service line is to expand the COPD clinical pathway to more patients.
“We have a nurse practitioner helping us with the high-risk COPD patients, but we’re not touching as many patients as we need to,” Dr. Collier said.
While readmissions have gone down, an important need is to reduce admissions from the Emergency Department. Identifying and aggressively treating COPD patients in the ED may spare patients the need for a hospital stay, she said.
“We are now shifting our focus to the transition points and primary care settings, identifying drivers for COPD admissions and re-admissions, and working to optimize care across a broader continuum,” said Vinay Maheshwari, M.D., MHCDS, FCCP, associate chair of Specialty Medicine, Department of Medicine, associate physician operations lead for the service line and director of Intensive Medicine.
Additionally, Acute Medicine is working on strengthening its smoking-cessation program and continuing to place patients into pulmonary rehab.
“Smoking cessation and pulmonary rehab have the most important impact on their quality of life,” Dr. Collier said.
Behavioral Health: Suicide assessment
The newest clinical pathway for the Behavioral Health service line addresses a leading cause of preventable death: suicide.
Three times as many Americans die from suicide than homicide, according to a 2014 report from the Centers for Disease Control and Prevention.

“It’s a huge public health problem,” said Linda Lang, M.D., chair of Psychiatry and service line physician leader. “The rate is higher now than it was 10 years ago. It’s getting worse, and we have to do something about it. We felt it was our role at Christiana Care to take this on.”
The pathway involves incorporating the Columbia Suicide Severity Rating Scale (C-SSRS) into Christiana Care’s electronic medical record system.
The scale, developed by psychologists at Columbia University, uses six questions to gauge if a person is suicidal. Embedding the scale in standard operating procedures will help clinicians identify suicidal patients who are admitted with unrelated health issues like diabetes or high blood pressure. One of the advantages of using the C-SSRS is that it can be administered by anyone, regardless of medical training.
“Some patients who might not admit to feeling suicidal upfront may open up when someone is sitting with them asking questions from the Columbia scale,” Dr. Lang said.
The pathway also calls for educating staff so they know what signs to look for in suicidal patients. Statistics show that 45 percent of people who commit suicide were seen in a primary care office within 30 days of their death, she said.
Implementation of the pathway is occuring in phases. The Columbia scale has already been rolled out for inpatients. Eventually all patients will be screened.
In the hospital, many resources are required to care for suicidal patients — for example, “safety sitters” — staff who watch over patients. Being able to stratify the risk will enable the hospital to deploy its resources most efficiently, she said. Depending on their risk — low, moderate or high — patients will be offered treatment ranging from education to inpatient care.
The suicide assessment initiative complements the service line’s inaugural clinical pathway, which standardized the screening, identification and treatment of patients at risk for opioid withdrawal.
“One-third of people who commit suicide have a substance-abuse problem,” she said. “The pathways are very linked.”
The service line established a screening tool for opioid use similar to the one being used to assess suicide risk. At the time, they predicted that the clinical pathway would reveal that between 2 and 10 percent of patients being admitted to the hospital are in opioid withdrawal. Early results suggest that 2 percent of admissions are in active withdrawal, Dr. Lang said.
“We are learning that patients coming in with an infection such as pneumonia may also be experiencing heroin withdrawal,” she said. “Once the withdrawal symptoms emerge, they want to leave or sign out against medical advice, and they leave with untreated infections. By treating their withdrawal, we should start to see AMA rates going down and improve the overall health of the community. Many of them have been willing to accept help in community-based drug programs.”
Cancer Care: Supportive care of oncology patients
The Cancer Care service line is adopting a new clinical pathway that aims to improve the quality of life and health outcomes for certain patients receiving multiple modes of treatments at once, like chemotherapy and radiation.
“We discovered looking back that our high 30-day readmission rate is with these patients,” said Nicholas Petrelli, M.D., Bank of America endowed medical director of the Helen F. Graham Cancer Center & Research Institute and physician leader for the service line. “These patients are readmitted for dehydration secondary to their treatment.”
The clinical pathway is focused on patients with cancer located in the head, neck, thoracic or rectal areas.
The new protocol is called SCOOP, or supportive care of oncology patients, said Chris Koprowski, M.D., MBA, associate physician leader of the service line.
The idea, he said, is to provide the same supportive, early intervention to patients being treated curatively as the palliative care afforded those with advanced disease. He cited a Harvard University study showing that patients receiving such care early-on lived longer and enjoyed a better quality of life.
“I predict we will impact our patients in terms of improving their quality of life and patient experience,” he said. “It’s fairly unique. There was next to nothing written about this particular approach when we reviewed the literature.”
Dr. Koprowski estimated that about 100 patients will be touched by SCOOP in its first year. Those identified for the pathway will have their needs tracked in the areas of social work, nutrition and behavioral health. If a patient does end up in the Emergency Department, he or she will be identified and admitted directly to a cancer floor, and the patient’s care team will be alerted upon discharge.
“We have baseline data on these folks that is relatively reliable,” Dr. Koprowski said. “We’d like to see diminished emergency room visits, diminished admissions and readmissions, and greater patient satisfaction,” he said.
In part, the service line plans to reduce readmissions by providing a medical support “home” staffed by a primary care physician, where patients can be treated instead of being admitted to the Emergency Department.
Meanwhile, Dr. Petrelli said, the service line’s first clinical pathway has proven a success. It zeroed in on patients with operable Stage 2 non-small-cell lung cancer. The service line leaders chose this patient population because it was a small group that would be easier to track. So far this year, there are 13 patients enrolled in the pathway.
“We’re measuring whether they receive surgery or not, chemotherapy; we are closely watching to ensure there are no unnecessary scans or unnecessary treatments, and that they are following up with their primary care physician,” said Tammy Brown, RN, MSN, OCN, NTABC, clinical director of the Cancer Program.
“We have 100 percent compliance,” Dr. Petrelli said. “We don’t seem to have an inappropriate use of PET scans.”
Heart and Vascular: Syncope
The Heart and Vascular service line has chosen for its second clinical pathway a common condition with a variety of causes: syncope, or loss of consciousness.

“One of the bigger problems we have today is we have many people with syncope getting too extensive a workup,” said Timothy Gardner, M.D., physician leader of the Heart and Vascular service line and medical director of the Center for Heart & Vascular Health. “You wouldn’t want someone who is otherwise healthy to go through an extensive neurological workup, just like you wouldn’t want someone who has a low likelihood of a heart rhythm problem to wear a 24-hour heart monitor for a week.”
Emergency room physicians, who see hundreds of patients a day, understandably are concerned about missing something life-threatening, he said.
“The tendency is to over-test, but if we can develop evidence-based practices to treat patients more effectively, more safely and lower the cost — that’s the holy grail to reducing unnecessary testing and treatment,” he said.
In many cases, a fainting spell is caused by conditions fairly simple to treat. The patient could be dehydrated, anxious or have forgotten to take their blood pressure medicine.
“Patients who have syncope don’t have an obvious diagnosis,” he said. “We get a large number of patients who get admitted with a syncopal diagnosis, and most of them get admitted on observation status.”
In the past 18 months, Christiana Care has treated 2,800 patients — or 156 per month — for syncope. About 60 percent were discharged from the Emergency Department, Dr. Gardner said.
Syncope can be a sign of a more serious problem, like a heart blockage or a neurological issue. But because of the wide variety of potential causes, the possible pathways for treatment are varied.
“Obviously, some people with syncope do have serious causes, especially older people, so we need to both reduce variation and be effective,” he said.
First, a physician will make sure there are no injuries associated with the episode, like a fall. The patient’s medical history will be reviewed with an eye toward obvious explanations such as medication. In rare instances, if there are other symptoms indicating there might be something wrong with circulation to the brain, the patient will be targeted for a neurological workup.
Even for patients who need further evaluation, a hospital stay isn’t necessarily the most appropriate option. If, for example, the patient can be seen the following day by a cardiologist, he or she wouldn’t have to be admitted to the hospital.
In its first clinical pathway, the Heart and Vascular service line addressed the most common type of heart attack: the non-ST-segment-elevation myocardial infarction, or NSTEMI.
Christiana Care sees about 50 NSTEMI patients per month, most of whom are identified in the Emergency Department. The clinicians there now consistently use a scoring system known as thrombolysis in myocardial infarction (TIMI) that predicts which patients are of highest risk. The workflow also determines the frequency of troponin tests.
“Developing the NSTEMI clinical pathway was really a wonderful experience,” said Leslie Mulshenock, MBA, director, Heart and Vascular, Business & Informatics, and administrative project lead for both clinical pathways. “We’ve had a slight reduction in length of stay, and medication compliance is up.”
Dr. Gardner concurred. “I’m very pleased with the initial implementation of the NSTEMI clinical pathway. For patients who have come through the Emergency Department and were diagnosed early-on with NSTEMI, we’re getting tremendous compliance and participation.
“It’s been especially helpful in reducing time spent in the emergency room, and the coordination between emergency room staff and cardiology has been greatly improved.”
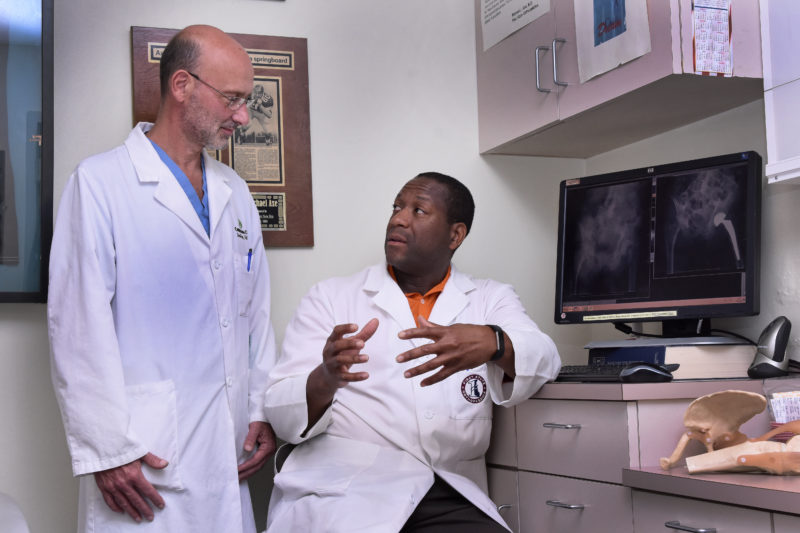
Musculoskeletal Health: Hip FIT (Fracture Intervention Team)
If the Musculoskeletal Health Service Line’s new Hip FIT (Fracture Intervention Team) clinical pathway is successful, its physicians will never meet the people they’ve helped the most.
That’s because the population will become educated at an earlier age about the importance of maintaining bone health and won’t need their services.
“A primary goal of the Musculoskeletal Service Line is to improve the bone health of our neighbors,” said Brian Galinat, M.D., MBA, physician leader for the service line and chair of the Department of Orthopaedic Surgery. “The more awareness people get regarding their bone health when they are in their 20s, 30s, 40s and 50s, the fewer hip fractures we will see in older folks.”
Christiana Care treats more than 500 hip fracture patients each year. Regardless of age, it’s always a severe injury.
The pathway establishes better coordination of care for patients with hip fractures. Dr. Galinat believes the new protocol will decrease length of stay, and Christiana Care’s care-coordination and support platform should help decrease readmissions.
Standardizing the treatment plan also better positions Christiana Care with Medicare’s bundled payment program — a new payment model that incentivizes health care providers to improve quality and health outcomes while reducing cost.
“This is an opportunity for us to do the right thing and benefit from a new payment model that was spawned by the Affordable Care Act.” Dr. Galinat said.
The new clinical pathway aims to reduce the time between a patient’s arrival and surgery by utilizing only the medical consults that are appropriate for each patient. “For example, clinical decision guidelines will allow the hospitalists to clearly know when and when not to consult cardiology. If we can safely get the patient to the operating room in under 36 hours, we will have better patient outcomes,” he said.
The protocol also engages social services earlier in the process to help a family select a proper skilled nursing facility earlier so that discharge is not delayed. “Interestingly, patients admitted with a hip fracture on the weekend currently have an overall shorter length of stay. We are fairly sure that this is in large part to issues related to transfer to skilled facilities on a weekend. If you come in on a Saturday, you may leave Wednesday. If you come in on a Tuesday, you may leave Monday.”
The Musculoskeletal Health Service Line learned a lot from its first clinical pathway, vertebral fragility fractures, he said. So far, that pathway has enrolled about 115 patients.
The pathway for vertebral fragility fractures consists of two main components: coordinating follow-up care to ensure patients are connected with an osteoporosis provider who can guide them through treatment to prevent future fractures, and narrowing spine surgery consults to the minority who might benefit from them.
Dr. Galinat said future clinical pathways, like the present ones, will carry a unifying message of the importance of bone health.
“As long as we keep this the focus of the Musculoskeletal Health Service Line, providers from pediatrics to primary care will take more time to make bone health a part of the discussion,” he said. “It will have a trickle-down effect throughout the health system and our community.”
Neurosciences: Uncomplicated seizure
For its second clinical pathway, the Neurosciences Service Line wanted to focus on a population best served in an outpatient setting — people presenting to the Emergency Department with an uncomplicated seizure.
“Many of these patients do not require admission to the hospital if they can be set up with rapid follow-up care in the outapatient setting,” said Valerie Dechant, M.D., associate service line leader and medical director of Neuro Critical Care. “The uncomplicated seizure clinical pathway focuses on facilitating patients’ access to neurological services. If they come to the Emergency Department, whether with their first or breakthrough seizures, we focus on connecting the patient to the appropriate resources in the community. This creates a better experience for the patient and more appropriate utilization of resources for the health system.”
In addition, she said, Christiana Care is hiring more epilepsy experts as part of a plan to develop a dedicated epilepsy center.
Dr. Dechant estimated that anywhere from 200 to 300 patients will be enrolled in the new clinical pathway in the first year.
The target group will be patients 18 and older who are not pregnant and whose seizures are not due to conditions such as acute trauma, infection, stroke, or alcohol or drug use, said June Wang, M.D., Ph.D., an epileptologist who practices with Christiana Care Neurology Specialists. Every day, the Emergency Department sees several patients who have had seizures due to a variety of reasons — maybe they haven’t taken their medication appropriately, or are suffering from sleep deprivation or stress, or their medications need to be adjusted, she said
“We want to have a standardized care plan in the emergency room so everybody will be on the same page,” Dr. Wang said. “We want to avoid unnecessary testing and admission.”
The major improvement the new pathway will provide is a better transition from the Emergency Department to outpatient services.
“Currently, after a visit to the emergency room, there is a disconnection in how you continue the care,” she said. “There really is a big gap between the emergency room and outpatient clinics.”
Under the new protocol, information about every patient in the pathway will be sent to an outpatient clinic. Dedicated staff will review the database each morning and discuss a treatment plan with a medical provider. The pathway also will capture new patients with a diagnosis of epilepsy who aren’t yet connected with specialty care.
“This is the time we can find those patients and avoid the burden of unnecessary admission in the future,” she said.
Meanwhile, the service line’s first clinical pathway, treating patients for acute ischemic stroke, has been going well, Dr. Dechant said.
“We rolled out several information technology aids that have really helped us get our patients on the pathway, track what we’re doing with them and make sure they are getting the services we want them to get,” she said.
Clinicians check up on the enrolled patients on a monthly basis. In addition, the standardized order template for stroke patients points them toward getting the proper medication.
“That guide ensures these patients get the rest of the pathway applied,” Dr. Dechant said. “We continue to gain momentum in people using that tool, and that speaks to the fact that not only is it good for the patients, but it is user-friendly for the doctors. People have really embraced the idea.”

Primary Care: Practice transformation
Every one of the 110,000 patients treated by the Primary Care & Community Medicine Service Line will be touched by its new clinical pathway: practice transformation.

“We use it as a catch-all term to encompass a range of practices we need to undertake, rather than choosing to focus on one disease,” said Omar Khan, M.D., medical director for Community Health at the Eugene du Pont Preventive Medicine and Rehabilitation Institute and service line physician leader. “With 30 to 50 common diseases, if we attacked everything on a disease basis, it would take us quite a while. What we really needed to do was install broad-based intervention. It was ‘go big, or go home.’”
If that sounds like a heavy lift, that’s because it is. But the service line already has made great strides, thanks to a team effort.
“Our colleagues from across the service line and medical group deserve a great deal of credit,” Dr. Khan said.
The goal is to certify all of the health system’s primary care sites as Patient-Centered Medical Homes, as deemed by the national Center for Quality Assurance, by mid-2018, he said.
In 2011, Christiana Care’s Department of Family and Community Medicine became the first practice in the state to earn that distinction (Level 1 of 3).
This past summer, two other practices — Wilmington Health Center’s Adult Medicine and Pediatrics —received Level 3 certification, a step up from the Level 2 accreditation it earned in 2013.

“It was a large push to get that group re-certified, and that was successful,” said Julie Silverstein, M.D., FACP, associate service line leader for Primary Care & Community Medicine.
The team effort included Nancy Howard, MSM, FABC, director of Primary Care Operations; Mary Ann Faralli, Ed.D, MSN, MBA, RN, CCRN, Quality Improvement Program manager; and Sarah Schenck, M.D., FACP, medical director for Adult Medicine, and care coordinator Crystal Pollock, RN-BC, both at the Wilmington Hospital.
“It’s a very strong team, and they have been working hard to assess practice needs and identify gaps,” Dr. Silverstein said.
The challenge, she said, was not so much in improving practices, but documenting standards that Christiana Care already has in place to demonstrate their qualification for the certification.
“The biggest reward was reviewing national standards and recognizing that we were adhering to those standards already. Some of it was out of organic growth, doing what we knew was right and providing the type of care we want to provide.”
To achieve certification, facilities need to document that they use patient-centered practices and provide coordinated care.
“You have to show evidence that you’re doing certain things — you’re patient-friendly, accessible and delivering care as the patient wants it. It’s transforming the practice into a basket of services that really wraps itself around the patients’ needs,” Dr. Khan said.
For example, a phone is the best technology that some patients have. “Our technology has to be what the patients are also using. If they call an office with a concern, the priority should be to get them seen by a primary care physician that same day,” he said. “It should be seamless customer service from entrance to exit.”
The initiative is boosted by a state innovation model (SIM) grant from the Delaware Center of Health Innovation. It also is supported by a partnership between the Delaware Academy of Family Physicians and its counterpart in New Jersey, which together are overseeing the Practice Transformation Services Project.
“This certification is far more than just a stamp of approval,” Dr. Khan said. “What it signifies underneath is that we’ve met very many metrics. The practice isn’t just the same practice with a new certificate. It is a practice transformed around patients’ needs.”
Meanwhile, the service line is doubling down on its first clinical pathway, which addresses the management of care for adults with Type 2 diabetes. The team is creating an online and smartphone-accessible module for diabetes management for providers in partnership with Endocrinology. Patients have access to the portal to transmit information such as blood sugar levels.
“A key opportunity for us was to allow a primary care physician to escalate medications for diabetes management in an appropriate manner,” he said. “Rather than having a consultation just for that, we can embed that information into an algorithm in a smartphone. It should save unnecessary complications and free up consultants for diabetes.”
The service line also is working on embedding key elements into patients’ electronic health records to help physicians decide on next steps.
Finally, Dr. Khan said, the department is piloting a shared visit concept for patients with equivalent conditions, to provide education and peer bonding.
Surgical Services: Perioperative evaluation and treatment services
Like their colleagues in Primary Care & Community Medicine, the Surgical Services team chose a clinical pathway that applies broadly across the service line, regardless of condition.

The subject, perioperative evaluation and treatment services, stemmed from the service line’s initial clinical pathway, recurring ventral hernia abdominal wall reconstruction, said Matt Rubino, M.D., FACS, chief of Surgical Services for Wilmington Hospital.
“We found out how important pre-operative optimization is,” Dr. Rubino said. “We realized we had the opportunity to make a big impact on a really broad patient population, regardless of what their diagnosis or surgery was.”
The trick is identifying high-risk patients whose surgical outcome can be improved by optimizing them before surgery, he said.
“There are certain high-risk patients who are going to be high-risk no matter what you do,” Dr. Rubino said. “We will be looking at different risk stratification tools to pick those patients out ahead of time. Part of that process is determining what outcome measures we want to look at — factors like length of stay, post-operative complications, readmissions, costs.”
Depending on patients’ co-morbidities, the service line will be looking at helping patients improve things like blood sugar level and body mass index. The goal is to provide care management on a continuum, from the time a surgery is scheduled to when the patient returns home.
“We’re still exploring different technologies for patient engagement,” he said. “How can we communicate more frequently and provide them with information?”
One resource will be CareVio, Christiana Care’s system for monitoring high-risk patients.
As for the current clinical pathway, the group has seen great improvements, said Joe Weiss, MHA, CHFP, CPHQ, administrative director for Perioperative Services.
The new protocol has shaved the average hospital stay from 11 days to seven or eight for the 80 recurring ventral hernia abdominal wall reconstruction patients enrolled in the clinical pathway, he said. That’s better for patients, and it also reduces the cost of care. Readmissions and emergency room visits also have gone down.
“We’ve had a quite few lessons learned over this process,” he said. “It’s very new working around the scheduling piece, reaching patients far enough out in advance. Instead of scheduling surgery in a week or two, we’re pushing it out to 30-plus days to optimize them,” he said. “We’re seeing some good traction with that, so it’s a big win for the team.”

Women & Children: TIME (Triple I to Manage Early Onset Sepsis)
The new clinical pathway being adopted by the Women’s and Children’s service line will reduce the number of healthy-term babies admitted to the neonatal intensive care unit, and will reduce unnecessary antibiotic treatment and separation of mothers and newborns.
The pathway standardizes the treatment of babies born to women with a condition previously called chorioamnionitis (commonly referred to as chorio) and standardizes treatment using “Triple I” criteria, which evaluates for the presence of intrauterine inflammation, infection or both to manage treatment.
Nationally, just 1 in 10,000 births will be affected by early-onset sepsis related to this diagnosis, and although rare, when it occurs, the results can be devastating.
“This is perfect subject matter for a new clinical pathway because there is not a standardized way for obstetricians to diagnose this on the maternal side,” said David Paul, M.D., physician leader of the service line and chair of Pediatrics.
Under current practice, all newborns of women with suspected chorio — regardless of whether they present with symptoms — are admitted to the NICU, where they are treated with intravenous antibiotics and stay for a minimum of 48 hours.
“This care of the newborn in the NICU requires the separation of mom and baby for something that’s unlikely to happen,” said Sherry Monson, RN, MSN, MBA, CENP, vice president of Women’s and Children’s Services.
To reduce the number of healthy-term babies admitted to the NICU, the service line will standardize maternal care of chorio using Triple I criteria and adopt the sepsis calculator tool by Karen Puopolo, M.D., PhD, et al to determine to treat in cases of suspected Triple I.
“It’s exciting to see the obstetricians, neonatologists, pediatricians and nurses from L&D, Mom-Baby and NICU all working together in a pathway that really affects the mom/baby dyad,” Monson said.
The service line will track the number of term babies admitted to the NICU, about 10 percent of whom are there for Triple I, to gauge the success of the pathway, Dr. Paul said. Specifically, the clinical pathway team aims to reduce by 20 percent the number of infants sent to the NICU because they were born to mothers with Triple I.
“This pathway fosters ‘TIME’ for mothers and babies to bond, reducing the anxiety of separation and improving the birth experience for many mothers whose newborn would historically have gone to the NICU to rule out sepsis,” said Linda Daniel, RN, MSN, CPHQ, director of Quality and Patient Safety for the Women & Children Service line. “A standardized approach will improve care delivery.”
The pathway calls for the babies assigned to a postpartum unit to have their vital signs monitored so that they may be treated quickly if they show signs of bacteria in the bloodstream, usually manifested in breathing difficulties.
“If the baby remains clinically healthy, we can skip a visit to the NICU,” Dr. Paul said.
Meanwhile, the Women & Children Service Line has seen its inaugural clinical pathway evolve, said Elizabeth Zadzielski, M.D., MBA, FACOG, medical director for ambulatory women’s health and associate leader of the service line.
That pathway focused on the treatment and follow-up care of gestational diabetes patients and their babies.
The new protocol increases compliance with gestational diabetes testing. Previously, women at risk of the condition underwent a one-hour test early in their pregnancy. An abnormal result would require them to return for a three-hour diagnostic test. That often meant a lag of one or two months, and only about 75 percent were following through with the testing, Dr. Zadzielski said.
In January, the service line adopted use of a two-hour screening and diagnostic test to eliminate the need for the initial one-hour test and subsequent three-hour test. Compliance continued to be an issue, so the team regrouped and have now integrated testing into an obstetrical visit for at-risk patients. Those mothers are now scheduled for an initial two-hour visit in which the test is administered, and the rest of the time is spent meeting with a nurse practitioner and nutritionist to provide education and counseling.
“Lo and behold, we found the patients really, really liked this — you can have important testing done and get some really useful education at the same time,” she said. “The upshot is that we’re actually looking to further partner with phlebotomy on-site.”
The intervention doesn’t stop there. Women who have gestational diabetes are at a high risk of developing Type 2 diabetes after delivery. But again, there was a low compliance rate in getting postpartum testing done six weeks after giving birth. New research indicates that there isn’t a difference in accuracy if a woman is tested directly postpartum or weeks later. Now, such at-risk mothers have their glucose tested before they are discharged.
“We have learned a lot,” she said. “The value of this pathway has been the opportunity for us to look at current processes and retool and realign to really deliver expert care.”



