Helen F. Graham Cancer Center hires pioneering scientific couple
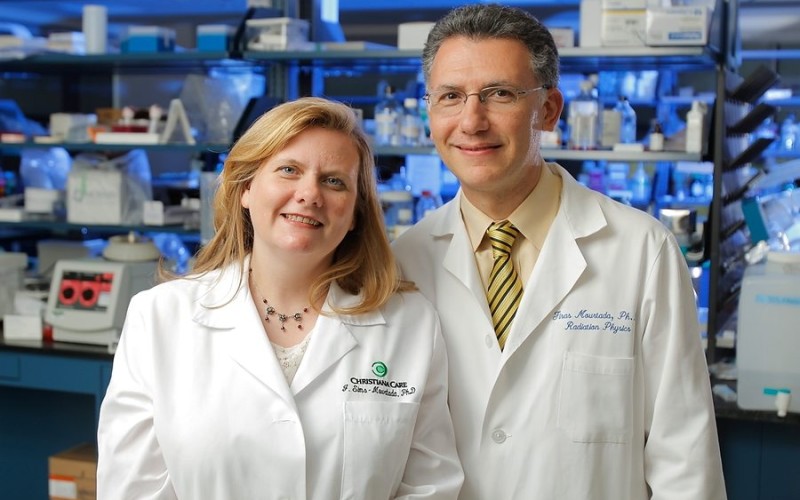
 With the hiring of two prominent scientists from the MD Anderson Cancer Center, the Helen F. Graham Cancer Center enriches both the translational cancer research and medical physics programs.
With the hiring of two prominent scientists from the MD Anderson Cancer Center, the Helen F. Graham Cancer Center enriches both the translational cancer research and medical physics programs.
Jennifer Sims-Mourtada, Ph.D., former director of Molecular research and Development, at radioMedix, Inc., in Houston and previously from the University of Texas MD Anderson Cancer Center (UTMDACC), is the Helen F. Graham Cancer Center senior clinical scientist for the Center for Translational Cancer research (CTCr).
Her husband, Firas Mourtada, M.S.E., Ph.D., D. ABr, is the new chief of Clinical Physics in radiation Oncology. Previously, Dr. Mourtada was a tenured associate professor in the Departments of radiation Physics and Experimental Diagnostic Imaging at UTMDACC. He retains an adjunct professorship with The University of Texas Graduate School of Biomedical Sciences.
Translational science
At the CTCr, Dr. Sims-Mourtada continues her pioneering work, investigating why some cancers are resistant to treatment and developing the imaging tools to target them for destruction.
“My goal is to find out which tumors would be resistant to treatment and which tumors are not likely to progress at all,” she says. The ability to characterize a patient’s tumor in this way would provide important information for doctors to prescribe the most effective course of treatment for individual patients.
Expert in radiation oncology physics
Dr. Firas Mourtada is an expert in radiotherapy physics, brachytherapy and dosimetry. He was on the faculty at UTMDACC since 2002. He holds several patents and has published and consulted extensively in the field of radiation oncology physics, contributing to best practice standards. As chief of Clinical Physics, he brings the unique perspective of a trained scientist as well as an experienced clinician to the Graham Center multidisciplinary cancer care team. He and his staff of dosimetrists and medical physicists, working with the entire radiation oncology team, play an important role in assuring accurate delivery of all aspects of the radiation treatment prescription.
One of Dr. Mourtada’s goals is to develop a medical physics residency training program and master’s degree program in medical physics at the Graham Center in the next few years. “Our efforts to establish a medical physics education program coupled with our leadership in patient care and research, I believe will solidify us as one of few, nationally recognized community hospital cancer centers,” he says.
All in the family
The Mourtadas’ passion for science brought them together 13 years ago. Their partnership has inspired creative approaches to solve some of the thorniest scientific questions about invading cancers and how to beat them.
Dr. Sims-Mourtada holds a Ph.D., in Biomedical Sciences from the Department of Immunology at The University of Texas Graduate School of Biomedical Sciences (2004). Her research on immune system genetics earned her a spot in the prestigious journal, Nature.
At radioMedix, Inc., (2006-2011), she built the company lab from the ground up and developed imaging agents for use with PET or CT scans. Under contract to the U.S. Defense Department, her group was the first to show that a radiolabeled protein called sonic hedgehog (named for a video game character) could differentiate stem cell-like breast cancer cells from other tumor cells, and potentially identify aggressive tumors. Her previous fellowship research in experimental radiation oncology at UTMDACC (2004-2006) was among the first to link hedgehog expression with resistance to radiation and chemotherapy.
Hedgehogs and tumor cells
“Given the successful tissue banking and procurement capability here at the Helen F. Graham Cancer Center,” she says, “I want to use the imaging techniques I’ve developed to go back and look at multiple aggressive tumor types for the sonic hedgehog signature.”
Unlike his wife, who is a Texas native, Dr. Firas Mourtada came from Syria. A new English speaker at 17, he studied biomedical engineering at Mercer University in Georgia. Upon graduation in 1992, he was one of 14 master’s degree candidates funded by the Whitaker Foundation Graduate Fellowship at The Johns Hopkins University in Baltimore, where he stayed to complete a Ph.D., in radiation Health (1997). After a one-year fellowship at the National Institute of Standards and Technology in Maryland, in 1998, he joined Guidant Vascular Interventions Corp., a Fortune 100 biotech company in Houston, as senior medical physicist. Over the next two years, Dr. Mourtada and colleagues developed a number of novel intravascular brachytherapy devices to treat cardiovascular disease.
At about this time, he met his future wife, Jennifer Sims. “I thought she was a brilliant scientist,” he recalls. The coupled married, and, in 2002, Dr. Mourtada joined UTMDACC as an assistant professor in the Department of radiation Physics. His biomedical engineering background and experience designing cardiovascular brachytherapy devices led to new collaborations that would benefit his cancer patients.
One example of his innovative work is a novel applicator for cervical cancer brachytherapy, which is expected to reach market in 2013. An unlikely partnership with scientists from Los Alamos National Lab produced an advanced dose calculation algorithm now used for planning external beam radiation and brachytherapy treatments. Dr. Mourtada contends, “If we are to eradicate cancer, we need to find ways to work together across all scientific disciplines.”
While at UTMDACC, Dr. Mourtada also served as an advisor to radioMedix, Inc., which afforded opportunities for the couple to work together. In 2011, the company earned support from the Texas Emerging Technology Fund to launch a novel device developed and tested in Dr. Mourtada’s lab at UTMDACC to radiolabel pharmaceuticals for PET imaging. The device potentially enables users to generate and label PET radiotracers on-site at much lower cost than those produced by current Cyclotron technology.